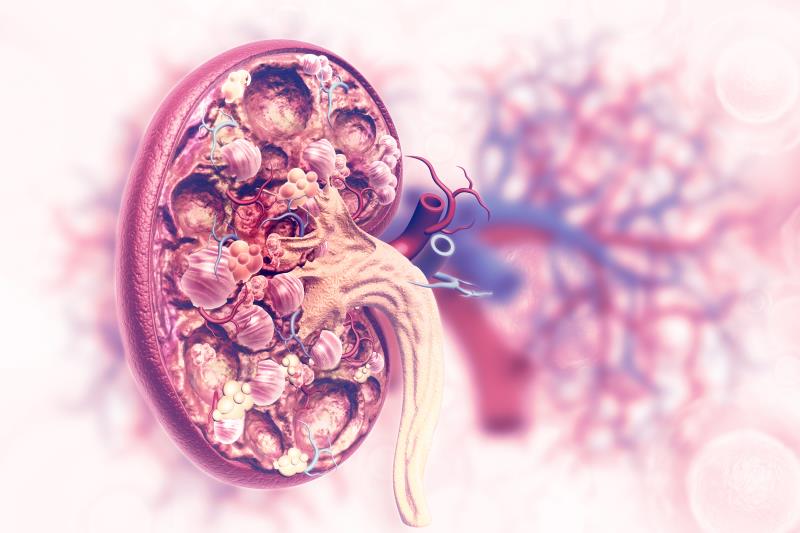
Percutaneous coronary intervention (PCI) appears to come with more complications in patients with connective tissue disease (CTD), leading to excess rates of acute kidney injury (AKI) and access site complications (ASC), a recent study has found.
Accessing the National Inpatient Database, researchers identified 17,422 CTD patients (mean age, 63.0±12.1 years; 63.2 percent female) who had undergone PCI between the years 2007 and 2015. Aside from AKI and ASC, other study outcomes included ventricular fibrillation, cardiogenic shock, stroke, in-hospital mortality and hospital length of stay (LOS). Patients were propensity-matched with 52,566 no-CTD controls.
AKI occurred significantly more frequently in the CTD arm than in controls (8.3 percent vs 6.6 percent; p<0.001), as did ASC (3.2 percent vs 2.7 percent; p=0.01). Mean hospital LOS was likewise significantly longer in patients with CTD (4.2±4.8 vs 3.8±5.2 days; p<0.001).
This was confirmed in multivariate analyses, which found that AKI was 18-percent more likely to occur in CTD patients (odds ratio [OR], 1.18, 95 percent confidence interval [CI], 1.01–1.27; p<0.001), while ASC was 14-percent more likely (OR, 1.14, 95 percent CI, 1.02–1.27; p=0.01). No such effect was found for the other endpoints.
Subgroup analyses yielded generally consistent results. AKI, ASC and hospital LOS were all significantly greater in patients with rheumatoid arthritis and systemic lupus erythematosus. In those with scleroderma, only AKI risk and LOS were elevated, while in patients with Sjögren’s syndrome, all three correlations were attenuated.
“Awareness of CTD diagnosis in patients before PCI could help operators apply caution in the volume of contrast used and make decisions about the duration and volume of hydration to decrease AKI. Also, such information may guide operators on the choice of vascular access and choice of vascular closure following PCI,” the researchers said.