A holistic approach to migraine management involves taking into consideration patients’ psychiatric comorbidities and addressing the cumulative burden of both diseases to help improve overall treatment outcomes. At an industry-sponsored symposium during the 2023 International Headache Congress in Seoul, South Korea, experts in neurology stressed the importance of bridging the gap between psychiatry and neurology in migraine care by highlighting the role of the calcitonin gene–related peptide (CGRP) pathway monoclonal antibody (mAb), fremanezumab, in migraine prevention in patients with comorbid major depressive disorder (MDD).
Psychiatric comorbidities common in migraine
“In migraine care, simultaneous screening for and assessment and management of patients’ comorbidities, specifically psychiatric disorders, are crucial because these are common in patients with migraine and can contribute to its burden,” said Professor Soo-Jin Cho of the Hallym University Dongtan Sacred Heart Hospital in Gyeonggi, South Korea. [J Headache Pain 2019;20:51; Headache 2012;52:1553-1565]
“Current evidence supports a bidirectional relationship between migraine and psychiatric comorbidities,” added Professor Piero Barbanti of the San Raffaele University in Rome, Italy. [J Headache Pain 2019;20:51] “For instance, patients with migraine are 4–5 times more likely to have generalized anxiety disorder [GAD], 2–4 times more likely to have depression, and about three times more likely to have sleep disorders.” [Neurol Clin 2019;37:631-649; Psychiatr Times 2013;30]
In a cross-sectional multicentre study, patients with headache and comorbid depression/anxiety were found to have an approximately 18 times higher risk of having poor or very poor quality of life (QoL) vs individuals with headache only. Patients with comorbid headache and depression/anxiety also reported worse outcomes in terms of work (eg, higher unemployment rates, less successful, reduced earnings), family/social relationships (eg, increased risk of feeling less understood by the family, employer and colleagues), and education (ie, increased risk of interference with learning), as well as increased healthcare resource utilization vs those with no psychiatric comorbidities. [J Headache Pain 2016;17:15]
“Stigma is a deeply discrediting attitude that is common towards both migraine and psychiatric disorders,” added Professor Gisela Terwindt of the Leiden University Medical Centre, the Netherlands. “In a population-based study of nearly 60,000 patients with migraine, approximately 32 percent experienced migraine-related stigma often or very often. This was associated with increased disability, increased interictal burden and poorer QoL.” [J Soc Work Values Ethics 2011;8:41-416; Shapiro RE, et al, AHS 2022, abstract IOR-03]
“Patients with mental disorders have been stigmatized across many cultures and societies,” said Barbanti.“Not only do stigmatizing attitudes against psychiatric disorders dramatically impact patients’ social life and self-esteem, but these also affect treatment-seeking behaviours that may concomitantly worsen outcomes.” [EMBO Rep 2016;17:1250-1253; Int J Environ Res Public Health 2019;17:280; J Clin Neurosci 2019;62:180-183]
“These observations show that psychiatric comorbidities are associated with worse migraine outcomes and a greater cumulative burden on patients,” he noted. [Gen Hosp Psychiatry 2014;36:533-538; Pak K Med Sci 2018;34:964-967; Cureus 2022;14:e25998]
CGRP pathway mAbs bridge the psychiatryneurology gap in migraine care
“Migraine has been proposed as a dysfunction of a neurolimbic pain network that shares similar neurotransmitters involved in the pathogenesis of psychiatric disorders [eg, serotonin, dopamine, glutamate, norepinephrine, and CGRP],” explained Barbanti. [Headache 2012;52:1553-1565; Int J Biomed Sci 2013;9:1-8; Ann Neurosci 2012;19:88-94; World Psychiatry 2010;9:155-161; Neurosci Lett 1994;182:138-142]
In particular, post-hoc analyses of randomized controlled trials (RCTs) have demonstrated efficacy of CGRP pathway–targeted mAbs (ie, erenumab and galcanezumab) in migraine prevention in patients with episodic migraine regardless of presence or absence of psychiatric comorbidities (ie, depression/anxiety). [Tepper S, et al, AAN 2018, abstract P4.105; Headache 2020;60:2202-2219] “This is an important observation because within the migraine population, patients with psychiatric comorbidities are considered as a difficult-to-treat [DTT] subgroup,” said Barbanti. [J Headache Pain 2022;23:56]
“There are also emerging reports indicating CGRP pathway mAbs’ efficacy in migraine treatment in people with depression,” continued Barbanti. [Psychiatr Pol 2022;56:711-728] “For instance, a real-world study retrospectively demonstrated high response rates associated with the CGRP mAb, fremanezumab, regardless of migraine type or presence of factors contributing to DTT migraine [ie, medication overuse, GAD, MDD, or prior exposure to a different CGRP mAb].” [J Headache Pain 2022;23:56]
“Since migraine and psychiatric disorders may have overlapping pathogenetic pathways, simultaneous treatments aimed at similar targets such as CGRP may be a prudent strategy,” he suggested.
UNITE: Fremanezumab in migraine prevention in patients with comorbid MDD
“Depression is prevalent in patients with migraine and is considered as a negative predictor of migraine treatment response,” noted Barbanti. [Lipton R, et al, AHS 2023, abstract P-231; Lipton R, et al, AHS 2023, abstract IO-05]
RCTs and real-world studies previously demonstrated efficacy and safety of fremanezumab in migraine prevention in adults. Fremanezumab is currently indicated for migraine prevention in adults with ≥4 migraine days/month. [JAMA 2018;319:1999-2008; Lancet 2019;394:1030-1040; N Engl J Med 2017;377:2113-2122; Neurology 2020;95:e2487-e2499; J Headache Pain 2022;23:47; J Headache Pain 2022;23:56; Ajovy Hong Kong Prescribing Information]
UNITE was a 12-week, multicentre, randomized, double-blind, placebo-controlled, parallel-group, phase IV study, followed by a 12-week open-label extension period, which aimed to evaluate the efficacy and safety of subcutaneous fremanezumab (monthly at 225 mg or quarterly at 675 mg) in adults (18–70 years of age; n=353) with both migraine and MDD. Eligible patients were adults diagnosed with episodic migraine (ie, headache >4–14 days/month, ≥4 of those migraine or required use of specific acute treatment) or chronic migraine (ie, headache ≥15 days/month, ≥8 of those migraine or required use of specific acute treatment) who had a history of MDD according to the Diagnostic and Statistical Manual of Mental Disorders 5th edition (DSM-V) criteria ≥12 months prior to screening with active symptoms of depression (ie, Patient Health Questionnaire-9 [PHQ- 9] score of ≥10 at screening). The primary endpoint was mean change in monthly migraine days (MMD) at week 12, while other key endpoints included change in MDD scores, responder rates, improvements in QoL and disability, and safety and tolerability. [Lipton R, et al, AHS 2023, abstract P-231; NCT04041284]
“UNITE is the first and currently the only RCT involving a CGRP-pathway mAb in patients with migraine and comorbid MDD,” noted Barbanti.
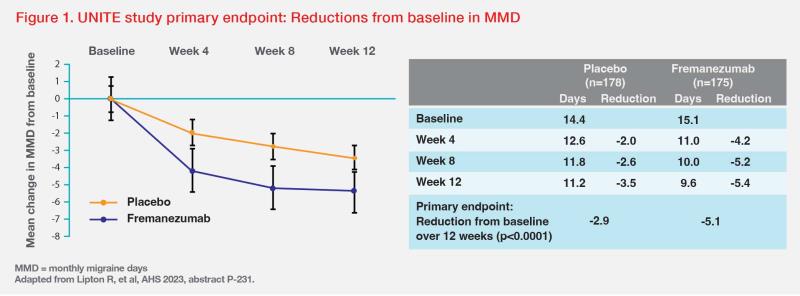
A total of 330 patients (fremanezumab, n=164) completed the doubleblind phase. Results showed significantly greater reductions from baseline in MMD in the fremanezumab vs placebo group after 12 weeks. Mean change from baseline in MMD during the double-blind period was -5.1 days vs -2.9 days for the fremanezumab vs placebo group (p<0.0001). (Figure 1) [Lipton R, et al, AHS 2023, abstract P-231]
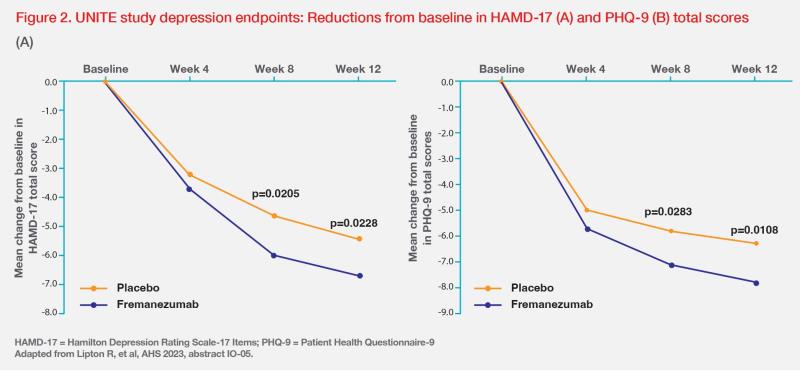
Patients who received fremanezumab also had significantly greater mean reductions from baseline in Hamilton Depression Rating Scale-17 Items (HAMD-17) total scores and clinically meaningful reductions in PHQ-9 total scores. For HAMD-17 scores, reductions in the fremanezumab vs placebo group were -6.0 vs -4.6 at week 8 (p=0.0205) and -6.7 vs -5.4 at week 12 (p=0.0228). For PHQ-9 total scores, reductions were -7.1 vs -5.8 at week 8 (p=0.0283) and -7.8 vs -6.3 at week 12 (p=0.0108). (Figure 2) [Lipton R, et al, AHS 2023, abstract IO-05]
Adverse events (AEs) were reported in 40 percent vs 27 percent of patients in the fremanezumab vs placebo group. The most common AEs were infections and infestations (15 percent vs 10 percent) and injection-site reactions such as pain, pruritus and oedema (11 percent vs 5 percent). [Lipton R, et al, AHS 2023, abstract P-231]
Importantly, these efficacy and safety results were maintained throughout the open-label period. [Lipton R, et al, AHS 2023, abstract P-231; Lipton R, et al, AHS 2023, abstract IO-05]
“Individuals with both migraine and depression represent a high-risk and complex population and are considered as DTT patients,” emphasized Barbanti. “Results from UNITE underscore fremanezumab’s efficacy and tolerability in both migraine prevention and improving MDD symptoms, which may help reduce the cumulative burden in patients with both debilitating conditions.” [Lipton R, et al, AHS 2023, abstract P-231; Lipton R, et al, AHS 2023, abstract IO-05]
Summary
“Psychiatric comorbidities are common in patients with migraine, resulting in higher cumulative burden that may worsen treatment outcomes,” said Barbanti. “Results from the UNITE study highlight the efficacy and tolerability of fremanezumab in preventing migraine and improving MDD symptoms, which suggest that CGRP pathway mAbs may have a role in helping bridge the gap between psychiatry and neurology in migraine care.”
This special report is supported by an education grant from the industry.