Sodium-glucose cotransporter 2 (SGLT2) inhibitors’ (eg, empagliflozin) cardiorenal benefits demonstrated in patients with type 2 diabetes mellitus (T2DM), heart failure (HF) and chronic kidney disease (CKD) have led to guideline recommendations for their use across these populations. In a Boehringer Ingelheim–sponsored lecture at the 6th Annual Meeting of Endocrinology, Diabetes & Metabolism Hong Kong (EDM HK), Professor Dirk Müller-Wieland of the RWTH University Hospital Aachen in Aachen, Germany, discussed how these cardiorenal-protective therapies improve patients’ prognosis, highlighting international guidelines that now recommend SGLT2 inhibitors for cardiorenal risk reduction in T2DM patients with atherosclerotic cardiovascular disease (CVD), HF patients regardless of left ventricular ejection fraction (LVEF) and diabetes status, and CKD patients.
New paradigm in diabetology & cardiorenal medicine
“Given SGLT2 inhibitors’ cardiorenal benefits in T2DM, HF and CKD, it is now important to risk-stratify patients and offer these organ-protective therapies to those at risk of complications or disease progression, in order to improve their prognosis,” said Muller-Wieland.
SGLT2 inhibitors’ cardiorenal benefits
“The EMPA-REG OUTCOME trial was a game changer in diabetology, demonstrating significant relative risk reductions [RRRs] with empagliflozin vs placebo in the primary outcome of 3-point major adverse CV events [MACE; ie, CV death, nonfatal MI or nonfatal stroke] [hazard ratio (HR), 0.86; 95.02 percent confidence interval (CI), 0.74–0.99; psuperiority=0.04], as well as in CV death [HR, 0.62; 95 percent CI, 0.49–0.77; p<0.001], all-cause mortality [HR, 0.68; 95 percent CI, 0.57–0.82; p<0.001] and hospitalization for HF [HHF; HR, 0.65; 95 percent CI, 0.50–0.85; p=0.002] in T2DM patients with established CVD, independent of HbA1c lowering,” Muller-Wieland highlighted. [N Engl J Med 2015;373:2117-2128] “CV outcome trials [CVOTs] of other SGLT2 inhibitors in T2DM patients also demonstrated similar RRRs in HHF.” [N Engl J Med 2017;377:644-657; N Engl J Med 2019;380:347-357; Circulation 2020;142:2205-2215]
Subsequent chronic HF trials in patients with or without T2DM demonstrated significant benefit with SGLT2 inhibitors across a wide spectrum of LVEF. [N Engl J Med 2019;381:1995-2008; N Engl J Med 2020;383:1413-1424; N Engl J Med 2022;387:1089-1098] In the EMPEROR-Reduced trial in patients with chronic HF with reduced ejection fraction (HFrEF) and the EMPEROR-Preserved trial in patients with chronic HF with mildly reduced or preserved ejection fraction (HFmrEF or HFpEF), for example, empagliflozin demonstrated significant RRRs in the primary endpoint of CV death or HHF vs placebo (EMPEROR-Reduced: HR, 0.75; 95 percent CI, 0.65–0.86; p<0.001) (EMPEROR-Preserved: HR, 0.79; 95 percent CI, 0.69–0.90; p<0.001). In both trials, empagliflozin’s benefits were consistent in patients with or without T2DM at baseline. [N Engl J Med 2020;383:1413-1424; N Engl J Med 2021;385:1451-1461; Circulation 2021;143:337-349]
“In patients with HFpEF or HFmrEF, SGLT2 inhibitors’ RRRs in CV death or HHF were consistent across LVEF categories, including LVEF ≥60 percent, according to a meta-analysis,” said Muller-Wieland. [Lancet 2022;400:757-767] “[The totality of evidence suggests that] all patients with symptomatic HF, regardless of LVEF, should receive SGLT2 inhibitor therapy.”
“SGLT2 inhibitors also demonstrated consistent RRRs in renal outcomes in T2DM CVOTs,” he continued. [JAMA Cardiol 2021;6:148-158] This laid the foundation for trials that evaluated their cardiorenal benefits in CKD patients with or without T2DM. Among these trials, the EMPA-KIDNEY trial of empagliflozin vs placebo enrolled the broadest range of CKD patients who were generally reflective of clinical practice, including patients with estimated glomerular filtration rate (eGFR) ≥20 mL/min/1.73 m2 and those with normal to moderately increased albuminuria. [N Engl J Med 2019;380:2295-2306; N Engl J Med 2020;383:1436-1446; N Engl J Med 2023;388:117-127]
“Although EMPA-KIDNEY’s population had lower risks of CV death and renal progression and the trial’s follow-up duration was shorter, RRR in the primary composite outcome was comparable to that observed in CKD trials of other SGLT2 inhibitors,” pointed out Muller-Wieland.
After 2 years of follow-up, empagliflozin demonstrated a 28 percent RRR in the primary outcome of kidney disease progression (ie, end-stage kidney disease, sustained decrease in eGFR to <10 mL/min/1.73 m2, sustained decrease in eGFR of ≥40 percent from baseline, or death from renal causes) or CV death (HR, 0.72; 95 percent CI, 0.64– 0.82; p<0.001) vs placebo. [N Engl J Med 2023;388:117-127]
What do guidelines recommend?
Current international guidelines recommend SGLT2 inhibitors in T2DM patients at high cardiorenal risk, as well as in HF and CKD patients.
For T2DM patients with atherosclerotic CVD/indicators of high risk, HF or CKD, the American Diabetes Association (ADA) and European Association for the Study of Diabetes (EASD) recommend SGLT2 inhibitors with proven CVD or HF benefit or with primary evidence of reducing CKD progression, respectively, to reduce cardiorenal risk. [Diabetes Care 2022;45:2753-2786]
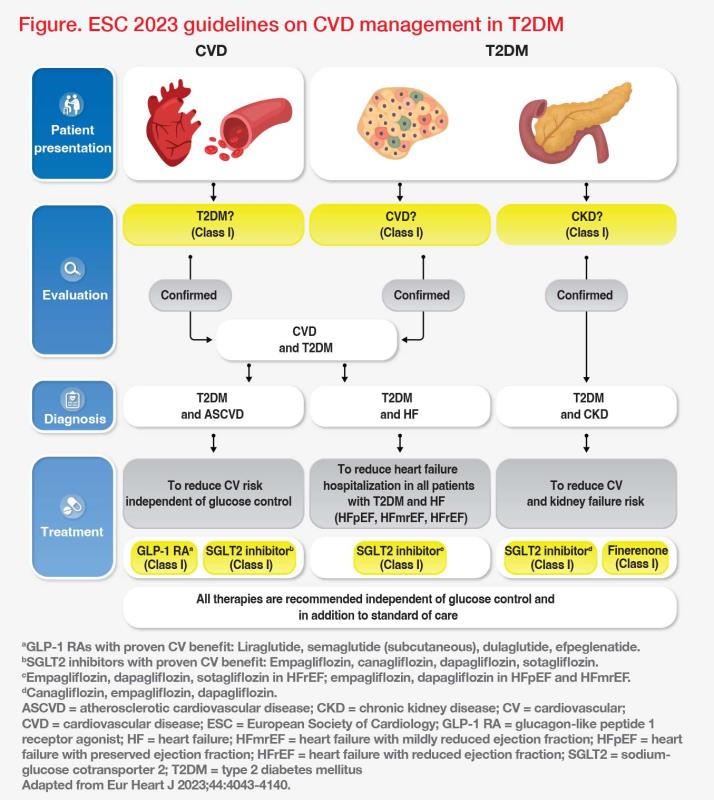
Similarly, the European Society of Cardiology (ESC)’s 2023 guidelines on CVD management in T2DM gave a class I recommendation for use of SGLT2 inhibitors in T2DM patients with atherosclerotic CVD, HF or CKD, to reduce their cardiorenal risk. “Of note, SGLT2 inhibitors are recommended independently of glucose control and regardless of concomitant standard medication in these patients,” pointed out Muller-Wieland. (Figure) “Glucose-lowering agents with proven CV benefit should be prioritized in T2DM patients with atherosclerotic CVD [class 1 recommendation].” [Eur Heart J 2023;44:4043-4140]
For patients with HFpEF, HFmrEF or HFrEF, ESC’s HF guidelines gave a class 1 recommendation for SGLT2 inhibitors as one of the first-line (1L) therapies for reducing HHF and/or mortality. [Eur Heart J 2021;42:3599-3726; Eur Heart J 2023;44:3627-3639]
“Given their HF benefits regardless of LVEF, SGLT2 inhibitors can be initiated in patients with symptoms of chronic HF, without waiting for echocardiography,” Muller- Wieland advised.
For patients with diabetic kidney disease, 2022 guidelines of Kidney Disease: Improving Global Outcomes (KDIGO) recommend SGLT2 inhibitors as 1L therapy if eGFR is ≥20 mL/min/1.73 m2. In these patients, SGLT2 inhibitors should be continued until dialysis or transplantation. [Kidney Int 2022;102:S1-S127]