Seeking GP’s proactive involvement in dispelling myths and promoting effective contraception
Senior Doctor
Family Planning Association of Hong Kong

In an interview with MIMS Doctor, Dr Grace Wong, Senior Doctor at Family Planning Association of Hong Kong (FPAHK), discussed main trends revealed in FPAHK’s Youth Sexuality Study 2021 and Hong Kong Family Planning Knowledge, Attitude and Practice Survey 2022, highlighting the importance of sex education and existing awareness gaps.
Contraceptive knowledge among youths and adults
FPAHK’s latest territory-wide Youth Sexuality Study, conducted in May–July 2021, surveyed 3,713 girls and 4,630 boys from Form 1–6. Results revealed a mean sexual knowledge score of 5.6 and 4.7 out of 12 among Form 1–2 girls and boys, and respective scores of 8.4 and 7.7 out of 12 among Form 3–6 respondents. [FPAHK, Youth Sexuality Study 2021]
“[Among youths], sexual knowledge improves with age, and the scores we see in Form 3–6 aren’t bad,” commented Wong. “However, two questions on contraception were answered correctly by less than half of respondents. These questions were on whether pregnancy can occur 2 weeks before menstruation or with extravaginal ejaculation.”
“Despite scoring relatively well overall, results of the survey indicate that respondents feel they do not have sufficient information,” shared Wong. “Indeed, sex education is not compulsory in Hong Kong. It is covered as part of values education along with other subjects, such as civic and national education, making the degree of emphasis on sexuality and contraception individual teachers’ choice.”
Leading sources of sexual knowledge among youths, as indicated by the survey, were teachers and social workers, friends and classmates, family members, Internet, and social media. “FPAHK has a wealth of educational resources [including a mobile classroom with audio-visual content and interactive games] and organizes workshops and youth volunteers’ training, which can hopefully discourage risk-taking behaviour and encourage use of contraception to prevent unintended pregnancy. In addition, we provide educational activity programmes upon individual schools’ requests,” explained Wong.
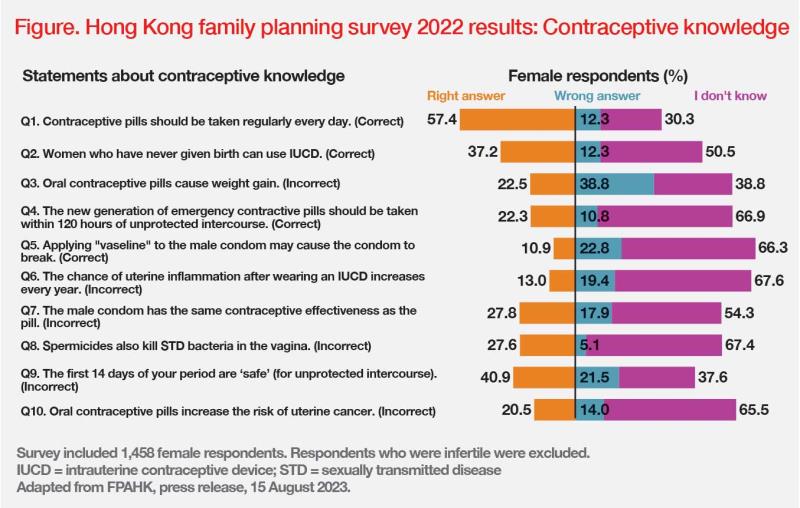
Of note, according to the results of FPAHK’s latest territory-wide Family Planning Knowledge, Attitude and Practice Survey 2022 among women aged 15–49 years and their spouses or cohabiting partners, both women and men showed poor contraceptive knowledge, on average respectively answering only 2.8 and 3.1 questions out of 10 correctly. Questions answered correctly by less than a quarter of female respondents involved correct use of the male condom, suitability and safety of intrauterine contraceptive devices (IUCDs), and oral contraception (OC) side effects. (Figure) Male respondents exhibited a similar lack of knowledge on these topics. [FPAHK, press release 15 August 2023]
Contraception in practice
Of the 1,458 fertile female respondents, 57.3 percent practiced contraception every time they had sex. The male condom was the most common principal contraceptive method (75.1 percent), followed by external ejaculation (8.5 percent), contraceptive pills (6.7 percent), IUCDs (3.9 percent), and injectable contraceptives (1.6 percent). [FPAHK, press release 15 August 2023]
“The combination of poor contraceptive knowledge, inconsistent use of contraception and growing use of less reliable conceptive methods, such as condoms and coitus interruptus, instead of pills and IUCDs, is somewhat disappointing, given FPAHK’s efforts in providing correct information and a variety of contraceptive services to the public,” commented Wong.
In the survey, 31.0 percent of female respondents reported having tried OC pills in the past, yet the proportion of current users was far lower, at 6.7 percent. “As OC is readily available in Hong Kong and does not require a doctor’s prescription, women may be unaware of OC’s minor, often short-term side effects, such as nausea and breast tenderness, which, if experienced, may lead some to assume that OC is not suitable for them and give up after a brief trial period,” explained Wong. [Hong Kong Med J 2016;22:231-236]
Emergency contraception pills: Area of concern
In the 2022 survey, 27.1 percent of female respondents indicated having ever used emergency contraceptive (EC) pills, with 4.9 percent reporting use in the past year. Of past-year users, 65.3 percent acquired EC pills from a pharmacy, 26.4 percent from a private doctor, 19.4 percent from FPAHK, and 6.9 percent from a Maternal and Child Health Centre. [FPAHK, press release 15 August 2023]
“Incorrect use of EC pills is common, as a majority of women buy them from drug stores, which may not even have a qualified pharmacist,” described Wong. “For example, a woman may take an EC pill a week after having had unprotected sex, by which point it may be ineffective, as it needs to be taken within 3–5 days of unprotected intercourse, depending on the type of EC pill. Some women may take an EC pill after missing their period, thinking it would act as an abortion pill. Women may not know that some EC pills may interact with regular OC. Some EC pills may affect the efficacy of regular OC, while the latest OC dose may also impair the efficacy of some EC pills.” [Faculty of Sexual and Reproductive Healthcare, Guideline on Emergency Contraception, July 2023]
Oral contraception: Advantages and safety considerations
“Although EC pills are an effective back-up, they are actually less effective than combined OC [reported failure rates with perfect use, 2–3 percent vs <0.5 percent],” noted Wong. [Lancet 2010;375:555-562; Cochrane Database Syst Rev 2013;2013:CD003552]
“As well as being one of the most effective ways to prevent unwanted pregnancy, OC also has a range of other advantages,” she continued. “Unlike condoms or surgical methods, OC is an intercourse-independent reversible form of birth control. OC’s noncontraceptive benefits include minimizing menstrual blood loss and pain, regulating the menstrual cycle and reducing acne.” [Hong Kong Med J 2016;22:231-236; Int J Womens Dermatol 2017;3:44-52]
However, FPAHK’s contraceptive knowledge quiz reveals two common misconceptions about OC, which may contribute to its relatively low use in Hong Kong. Only about a fifth of female respondents thought that OC pills do not increase the risk of uterine cancer or cause weight gain. (Figure) Although clinical literature suggests a slight increase in risk of breast and cervical cancers with combined OC pills, OC has protective effects in endometrial, ovarian and colorectal cancers. [Hong Kong Med J 2016;22:231-236]
“Another common concern expressed by women is risk of venous thromboembolism [VTE], which is not unfounded, particularly in smokers,” shared Wong. [BMJ 2013;347:f5298; Am J Hematol 2008;83:97-102] “Although VTE risk is generally lower among Asians vs Caucasians, at FPAHK, we provide individual and comprehensive risk assessment to select the most appropriate contraceptive method for all women who use our services.” [Prev Med Rep 2019;13:268-269]
“While VTE risk is higher in users of combined hormonal contraceptives vs non-users, failed contraception as a result of using less reliable methods can contribute to higher VTE risk when women are pregnant. Therefore, physicians should offer individual risk assessment, balancing the pros and cons, addressing women’s needs and concerns and correcting myths when providing contraceptive methods to women,” Wong suggested. [Aust Fam Physician 2016;45:59-64]