Successful use of r-FSH/r-LH combination in women aged ≥35 years with poor ovarian response
Specialist in Obstetrics and Gynaecology
Hong Kong

Case 1: A woman with unexpected poor ovarian response (POSEIDON Group 2)
A 39-year-old woman with an 8-year history of subfertility sought consultation in January 2022. She had regular menstrual cycles, and her BMI was 28 kg/m2. Her husband was diagnosed with mild teratozoospermia.
The patient had normal ovarian reserve, with antimüllerian hormone (AMH) level of 1.3 ng/mL and antral follicle count (AFC) of 6. During the follicular phase, her follicle-stimulating hormone (FSH) level was 9.2 IU/L and luteinizing hormone (LH) level was 3.6 IU/L.
In May 2022, the first controlled ovarian stimulation (COS) cycle using an antagonist protocol with 10 days of recombinant FSH (r-FSH; follitropin alfa, 300 IU) resulted in six follicles and retrieval of six oocytes. Three of these matured to become metaphase II (MII) oocytes, with one forming an embryo on day 3. Due to elevated progesterone level (5 pmol/L) during the COS cycle, the embryo was cryopreserved. Subsequently, frozen-thawed embryo transfer was performed in a hormone replacement therapy cycle. However, she did not conceive.
In view of poor ovarian response despite normal ovarian reserve, in September 2022, the patient received follitropin alfa 300 IU for 4 days, followed by 6 days of follitropin alfa/lutropin alfa 300/150 IU starting on day 5 of the second COS cycle utilizing an antagonist protocol. This cycle yielded seven retrieved oocytes, all of which reached MII. Two blastocysts formed on day 5 and day 6, respectively. After transfer of a frozen-thawed day-5 4AB blastocyst in next month, the patient became pregnant and delivered a baby.
Case 2: A woman with poor ovarian reserve (POSEIDON Group 4)
Following 3 years of subfertility, a 36-year-old woman sought consultation at our clinic in December 2022. She had regular menstrual cycles and normal BMI (22 kg/m2). Her husband was diagnosed with moderate teratozoospermia. Despite previously undergoing three cycles of ovulation induction and intrauterine insemination, the patient remained unable to conceive.
Baseline assessment showed AMH of 0.4 ng/mL and AFC of 3, with FSH level of 8.5 IU/L and LH level of 2.0 IU/L. It was concluded that the patient was a poor responder with diminished ovarian reserve.
In February 2023, 10 days of follitropin alfa/lutropin alfa 300/150 IU initiated on day 2 with the concomitant use of antagonist from day 5 of ovarian stimulation led to retrieval of four MII oocytes. Following transfer of a fresh 4BA blastocyst on day 5, the patient had a viable pregnancy.
Discussion
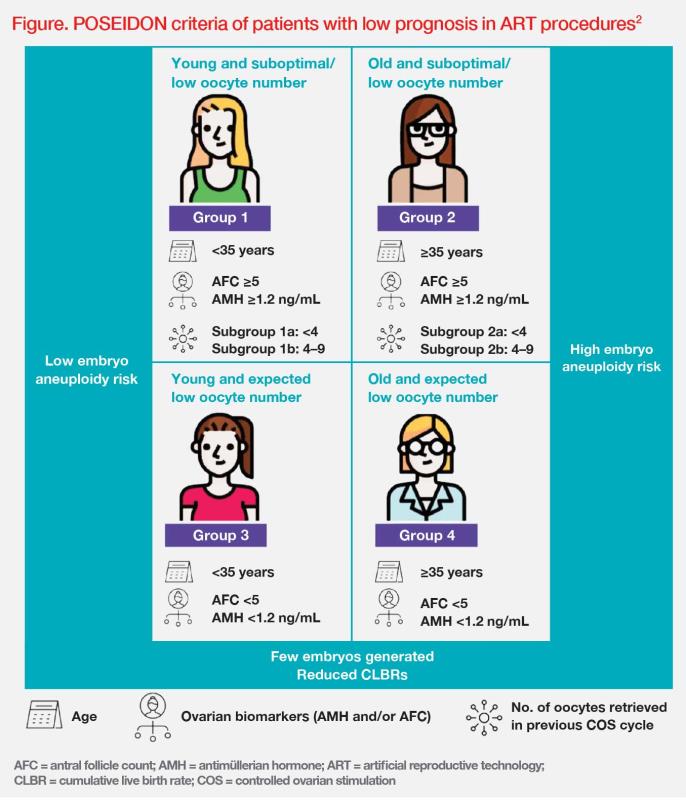
Poor ovarian responders are a heterogeneous population with diverse clinical characteristics. Classifying patients based on relevant parameters is important for tailoring in vitro fertilization (IVF) treatment strategies.1 The POSEIDON criteria propose utilizing ovarian reserve markers (AFC and/or AMH), maternal age, and the number of oocytes retrieved in the previous COS cycle to classify patients with low prognosis in assisted reproductive technology (ART) procedures.2 (Figure)
POSEIDON Group 2
POSEIDON Group 2 includes women aged ≥35 years with adequate AFC but deficient mature follicles, such as our patient in case 1.2 (Figure) This unexpected outcome could be due to suboptimal dosing of gonadotropins, genetic variants affecting endogenous expression of FSH or LH or their receptors, or technical issues during the IVF procedure.4
Recombinant LH (r-LH) supplementation may benefit women with poor response to exogenous gonadotropins in the prior COS cycle. A systematic review and meta-analysis showed that in women with unexpected poor ovarian response, use of r-FSH/r-LH combination was associated with higher number of retrieved oocytes (weighted mean difference [WMD], 1.98; p=0.03), higher implantation rates (odds ratio [OR], 2.62; p=0.004) and higher clinical pregnancy rates (OR, 2.03; p=0.003) vs r-FSH alone.5
Our patient in case 1 experienced ART failure after use of high-dose r-FSH in the first COS cycle. In the next COS cycle, r-LH supplementation resulted in an increased number of retrieved oocytes, ultimately leading to successful pregnancy and childbirth.
POSEIDON Group 4
POSEIDON Group 4 comprises women aged ≥35 years with low ovarian reserve, such as our patient in case 2.2 (Figure) In clinical practice, these poor responders often exhibit asynchronous or stagnant follicle growth. Because of substantial variations in follicle size during asynchronous follicle growth in COS, a considerable proportion of oocytes will fail to complete the maturation process, leading to poor outcomes.6 Pretreatments, which promote synchronization within the follicle cohort, such as oestradiol pill and/or r-LH/r-FSH combination, may be considered.7,8
rFSH/r-LH combination may enhance oocyte quality and ART outcomes in women at advanced maternal age. In a systematic review and meta-analysis, use of rFSH/r-LH combination was associated with improved clinical pregnancy rate vs r-FSH alone (OR, 1.45; 95 percent confidence interval [CI]; 1.05–2.00; I2, 0 percent; p=0.03) in patients aged 35–40 years. Despite fewer retrieved oocytes with r-FSH/r-LH vs r-FSH alone (WMD, -1.03; 95 percent CI, -1.89 to -0.17; I2, 0 percent; p=0.02), the number of MII oocytes remained comparable between two groups.9
Our patient in case 2 with a background of diminished ovarian reserve underwent ovarian stimulation with rFSH/r-LH combination. This cycle led to two fertilized oocytes, one of which further developed into a day-5 blastocyst. Our patient successfully conceived following fresh embryo transfer.
Furthermore, rFSH/r-LH combination can promote follicle growth and oestradiol production, supporting endometrial proliferation in women with hypogonadotropic hypogonadism.10 In women with profound LH suppression after gonadotropin-releasing hormone antagonist administration, r-LH supplementation may compensate for the suppressed LH levels.11 r-LH supplementation can also be effective in younger women with low baseline LH level (<1 IU/L). The failure of r-LH supplementation to increase pregnancy rate in women aged ≥40 years is likely due to high aneuploidy rates.9,12 It is important to engage in open discussion with patients and involve them in treatment planning for informed decision-making.
In summary, ART treatment strategies should be tailored based on patients’ profiles, especially after IVF failure. The above cases served as examples to illustrate that rFSH/r-LH combination may enhance outcomes by improving embryo quality and quantity in poor responders in their later 30s.