The coronavirus disease 2019 (COVID-19) pandemic is catalyzing the adoption of telemedicine in healthcare. MIMS Doctor examines the practical and medicolegal issues in this evolving field, and explores how barriers can be overcome to facilitate wider use of telemedicine for continuity and enhanced efficiency of care during the COVID-19 crisis and beyond.
Self-isolation, social distancing, lockdowns, and fear of contracting COVID-19 during healthcare visits have led to increases in requests for remote consultation and wider acceptance of telemedicine among both patients and healthcare providers. In Hong Kong, some centres, such as the CUHK Medical Clinic, have started providing remote consultation and COVID-19 screening in response to the unprecedented global health crisis.
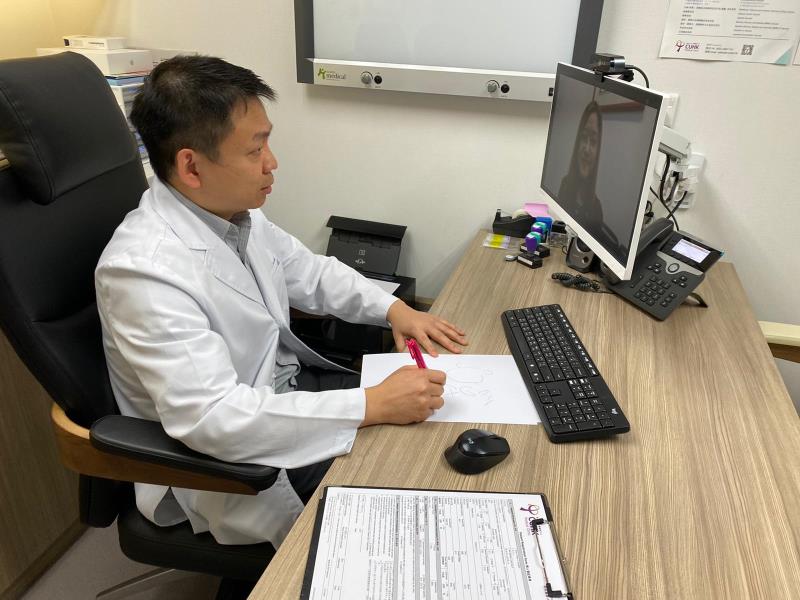
“Our telemedicine services, launched in early February 2020, are appreciated by patients for the convenience, efficiency and infection risk mitigation. These services have enabled us to maintain continuity of care during the COVID-19 pandemic,” said Dr Billy Chiu,Consultant / Senior Manager (Clinical Operation) of CUHK Medical Centre, in an interview with MIMS Doctor.
“As with traditional medical practice, it is important to be aware of the limitations and medicolegal issues, maintain a high overall standard of care, and align patients’ understanding and expectations of what telemedicine can and cannot provide,” said Chiu.
Medical Council guidelines: General principles
The Medical Council of Hong Kong (MCHK) Ethical Guidelines on Practice of Telemedicine, released in December 2019, define telemedicine not only as the provision of interventions, diagnoses, therapeutic decisions and treatment recommendations, but also the collaboration between doctors and/or with other healthcare professionals (HCPs), monitoring of patients, and dissemination of service information and/or health education to the public through telecommunication systems (including telephone, email and social media). [https://www.mchk.org.hk/files/PDF_File_Ethical_Guidelines_on_Telemedicine.pdf]
As with in-person consultations, doctors who practise telemedicine are held fully responsible for meeting all legal and ethical requirements, and are required to exercise due diligence. Well-established principles and standards of care for face-to-face consultations, including privacy and security of records, informed consent, safe prescribing and other key areas of medical practice, as set out in the MCHK’s Code of Professional Conduct, apply equally to telemedicine. [https://www.mchk.org.hk/english/code/index.html]
Importantly, doctors who treat or prescribe through telecommunication systems should ensure that they possess appropriate licensure in all jurisdictions where patients receive their medical services.
Telemedicine: For which patients?
“Provision of telemedicine services during the COVID-19 pandemic may come under the MCHK’s Code of Professional Conduct concerning serious infectious disease, which requires doctors to take adequate precautions when in contact with patients and medical specimens to minimize the risk of spreading infection to themselves and others,” said Dr Bobby Nicholas, Senior Medicolegal Adviser of Medical Protection Society (MPS), in a webinar for doctors in Hong Kong in March 2020.
The MCHK’s guidelines state that the practice of telemedicine is advisable only in cases with a prior in-person doctor-patient relationship. In cases where an existing doctor-patient relationship is not present, a doctor must take appropriate steps to establish a credible doctor-patient relationship, based on mutual trust and respect, with a patient before practicing telemedicine.
“This is relevant to COVID-19 screening, needed by a large number of patients, some of whom may not have a prior in-person relationship with a doctor,” said Chiu. “Some private doctors are providing remote COVID-19 screening using deep-throat saliva specimens to help alleviate the burden on the public healthcare system.”
“The rule of face-to-face consultation for first-time patients has been relaxed in the COVID-19 pandemic. Remote consultations can also be provided to new patients if it is safe to do so, and can be considered for use in all specialties, particularly in patients with chronic diseases,” said Dr Robert Hendry, Medical Director of MPS, in the webinar.
“Telemedicine services can be provided in cases where physical examination or contact is not required,” suggested Chiu. “The patient populations are therefore very broad, and not necessarily limited to those with chronic diseases or the elderly. It is applicable even in patients with inadequately controlled chronic diseases, if the patients are empowered and have good compliance.”
“In addition, triage calls can be utilized to understand patients’ presenting complaints prior to consultation, to enhance the efficiency of service,” Chiu added.

Considerations, caveats and special situations
According to the MCHK’s guidelines, telemedicine must not be viewed as a cost-effective substitute for in-person consultations. Any telemedicine service must be provided as part of a structured and well-organized system, with an overall standard of care comparable to service delivered otherwise.
“Before proceeding with a remote consultation, consider whether it is safe and reasonable to do so,” advised Nicholas. “Consider whether the patient’s identification is certain, whether the patient is able to identify the doctor, whether adequate medical records are available, whether the patient has consented to the mode of communication, whether the chosen medium for remote consultation is the most appropriate and technically sound, as well as data security.”
Adjustment of communication style
“Good communication, rapport between doctors and patients, and mutual trust and respect are as crucial for the practice of telemedicine as they are for traditional medical practice involving face-to-face consultations with patients,” said Chiu.
“Communication style should be adjusted during remote consultations to make sure patients understand the advice given. This is particularly important in telephone consultations, where nonverbal cues are missing,” he advised.
“It is also important to take into consideration the patients’ perceptions about their symptoms, even if their worries may be irrelevant to their conditions, and ask for patients’ feedback on the advice given to ensure compliance,” he added.
Record keeping, privacy and patient confidentiality
The MCHK’s guidelines state that doctors owe the same professional responsibilities with respect to medical record keeping and patient confidentiality in the practice of telemedicine as in in-person consultations. Data obtained during telemedical consultations must be secured through encryption, with other security precautions taken to prevent access by unauthorized persons.
“In the records, there should be a note that a remote consultation has been undertaken, with the rationale and content of the remote consultation clearly documented along with the advice given, follow-up plan and safety netting in case the patient’s condition changes,” advised Hendry.
Prescription and medication delivery
Some centres in Hong Kong are providing medication delivery on request following telemedicine consultation. While the MCHK’s telemedicine guidelines provide no specific guidance on medication delivery service, doctors are advised that prescribing via electronic means may be done only when they have adequate knowledge of the patient’s health and are satisfied that the medicine serves the patient’s needs, while considering the limitations of telemedicine, the need for physical examination or other assessments, and whether there is access to the patient’s medical records.
According to the MCHK’s guidelines, an in-person consultation is advisable before prescribing any medicine for the first time to a patient. When prescribing for an overseas patient, doctors should have regard to differences in a product’s licensed name, indications and recommended dosage regimen.
“Whether controlled drugs, such as hypnotics, can be prescribed in remote consultations is often determined by the facts of each individual case. Be very cautious, and consider whether there is appropriate and adequate information to justify the prescription of these medications,” advised Nicholas.
“Medication delivery by courier is generally not encouraged due to safety considerations, including reliability of the courier and the complexities of ensuring that the right medicines are delivered in intact form to the right patients,” noted Chiu. “At some centres providing medication delivery on request, it is the patients themselves who authorize a courier for medication pick-up and delivery.”
When to convert to in-person consultations?
“When physical examinations are necessary or likely to add critical information, patients should be advised to undertake in-person consultations,” said Chiu.
“Safeguarding concerns are also reasons for converting to face-to-face consultations or deferring a remote consultation to a more appropriate time, especially for vulnerable patients such as children, patients with psychiatric conditions, and the elderly,” suggested Hendry. “For example, consider who is in the room with the vulnerable patient, and whether the patient would be coerced inappropriately during the teleconsultation.”
“Inadequate medical records, technical limitations, and the possibility of potential confidentiality breaches should also prompt a face-to-face consultation or deferral of a remote consultation,” Hendry added.
Remote consultations for patients not in HK
“There have been increases in cross-border consultation requests from patients in mainland China in recent years. The current practice is for doctors in Hong Kong to provide advice to doctors in mainland China, for the doctors there to deliver care to the patients,” noted Chiu.
While the MCHK’s telemedicine guidelines do not provide very specific guidance about cross-border consultations, they do state that doctors working with or receiving reports from other HCPs should ensure that the required standards of care are followed, and should notify the other HCPs if there are concerns about the quality of care being provided. Furthermore, doctors who ask for another HCP’s advice or second opinion remain responsible for treatment, as well as other decisions and recommendations, given through them to the patient.
Beyond the COVID-19 pandemic: Breaking barriers in healthcare
“The COVID-19 pandemic has taken telemedicine a small step forward, but technical and regulatory limitations, as well as concerns among HCPs, remain as barriers to its wider adoption,” said Chiu. “The Hong Kong Telemedicine Association, established in recent years, is working towards overcoming these barriers to foster synergy in healthcare through telemedicine.”
“As big data and artificial intelligence [AI] are being rapidly developed in healthcare, further advances in telemedicine can be anticipated to improve the efficiency and accuracy of care,” suggested Chiu. “For example, these technologies can be utilized to build algorithms for more accurate history taking and diagnosis, and can also be applied in medical training.”
“Wearable devices can be used in telemonitoring of patients with chronic diseases, with data uploaded to a cloud platform for doctors to review before a follow-up visit. Algorithms can be built into these devices and platforms to prompt follow-up action when a patient’s condition changes,” he continued.
“Telemedicine is part of the overall drive for advances in health technologies, and is being developed in parallel with big data, AI, wearable devices and genomics. The ultimate goal of these developments is to provide better care to patients,” he concluded.