In an interview with MIMS Doctor, Dr Ka-Yuen Lock, Specialist in Endocrinology, Diabetes and Metabolism in Hong Kong, discussed management of diabetes mellitus (DM), including use of ultra-long-acting insulin, in optimizing glycaemic control. She also shared a case study illustrating improvements in glucose variability and patient’s satisfaction with insulin degludec (IDeg) in type 1 DM (T1DM).
Challenges of achieving good glycaemic control
“Hypoglycaemia is a major barrier to achieving tight glycaemic control in DM patients. Some patients, such as those with T1DM and those with type 2 DM [T2DM] on intensive insulin regimens or with a history of stroke, coronary artery disease and/ or renal failure, are at high risk of hypoglycaemia. In addition, patients with irregular lifestyles, including shift workers and frequent travellers, may have suboptimal adherence to insulin treatment, which leads to poor glycaemic control,” Lock said. [Curr Diabetes Rev 2013;9:195-208; Diabet Med 2012;29:682-689]
“For these patients, a once-daily regimen of ultra-long-acting insulin, which reduces hypoglycaemia risk, maintains a stable day-to-day glucose level and provides potential flexibility in the timing of administration, may improve glycaemic control and patients’ treatment satisfaction,” Lock continued. [Curr Diabetes Rev 2013;9:195-208]
Why ultra-long-acting basal insulin?
In T2DM patients, a single daily dose of basal insulin (eg, IDeg, insulin glargine [IGlar], insulin detemir [IDet], neutral protamine Hagedorn [NPH] insulin) is often used as the initial insulin regimen in addition to oral antidiabetic drugs (OADs). [Diabetes Care 2022;45(Suppl 1):S125-S143]
“IDeg and IGlar are commonly used basal insulin analogues that differ in their pharmacological properties. IGlar has a duration of action of 24–36 hours and a half-life of 12–19 hours. On the other hand, IDeg has a duration of action of >42 hours and a half-life of >25 hours, which allows some flexibility in its administration, requiring only a minimum of 8 hours between two sequential doses. IDeg’s pharmacological properties may benefit patients who have difficulties injecting basal insulin analogues at the same time every day,” Lock explained. [Cell Metab 2021;33:740-747; Diabetes Ther 2020;11:2539-2553; Tresiba Hong Kong Prescribing Information]
Use of IDeg across different DM populations
“In clinical trials and real-world settings, IDeg demonstrated a flat time-action profile and reduced risk of hypoglycaemia in DM patients,” Lock said.
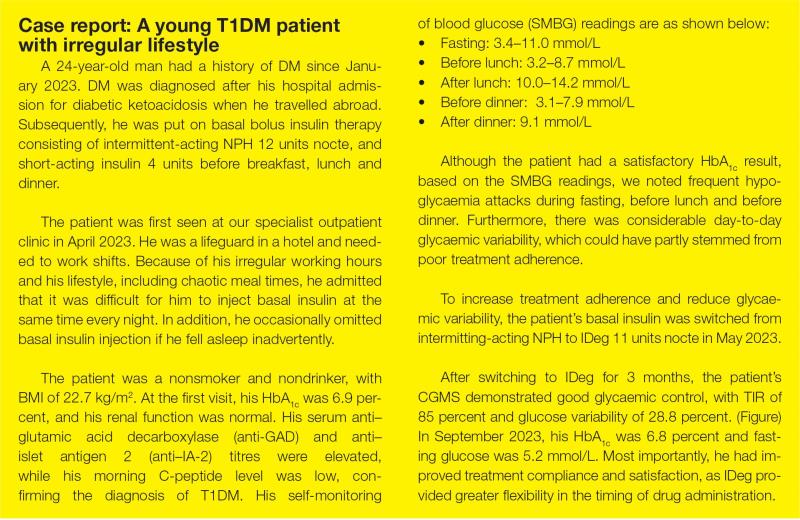
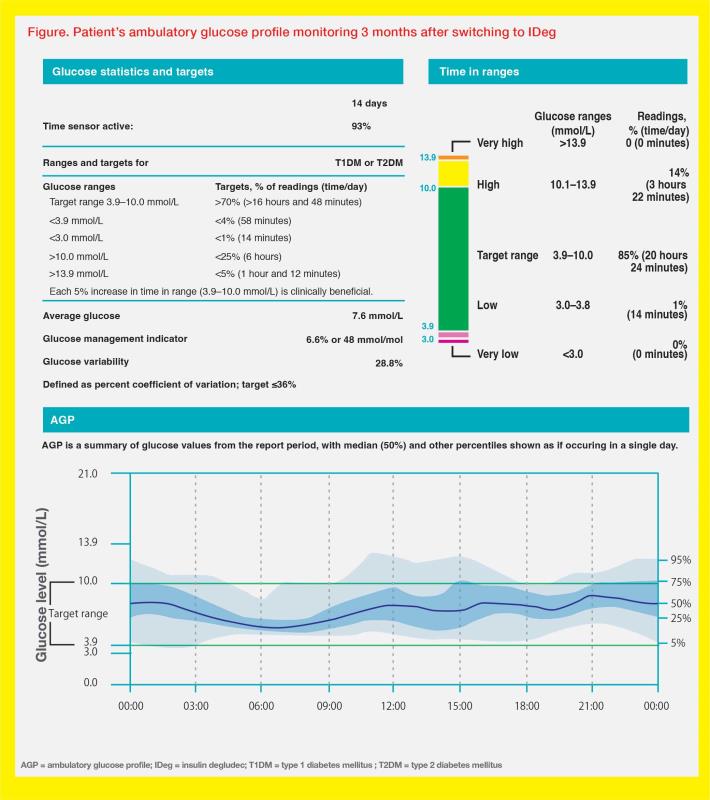
A crossover randomized controlled trial (RCT) in T1DM patients showed significantly less within-day and day-to-day variability in glucose infusion rate profiles with IDeg 0.4 U/kg vs IGlar U300 (both p<0.0001). In another crossover RCT involving T2DM patients with or without OADs, IDeg U100 increased time in range (TIR; glucose level 3.9–10.0 mmol/L) and reduced nocturnal time below range (glucose level ≤3.8 mmol/L) vs IGlar U100. [Diabetes Obes Metab 2017;19:1032-1039; Diabetes Obes Metab 2021;23:2572-2581]
The real-world, prospective, observational ReFLeCT study showed that a switch to IDeg from other basal insulin (eg, IGlar, IDet) was associated with lower rates of hypoglycaemia in T1DM patients (relative risk [RR], 0.28–0.90) and T2DM patients (RR, 0.54–0.56) during a 12-month follow-up period vs a 4-week baseline period. [J Clin Endocrinol Metab 2019;104:5977-5990]
Treatment with IDeg may also be considered in DM patients during pregnancy, if clinically necessary. [Tresiba Hong Kong Prescribing Information] The EXPECT study was an open-label noninferiority RCT involving 225 women with T1DM (mean age, 31.1 years; mean HbA1c, 6.7 percent) who were at 8–13 weeks of gestation or planned to become pregnant within 52 weeks. The study participants were randomized to be treated with IDeg or IDet in combination with prandial insulin aspart until 28 days after delivery or for up to 12 months if not becoming pregnant. Estimated mean HbA1c prior to delivery was 6.2 percent with IDeg and 6.3 percent with IDet (estimated treatment difference, -0.11 percent; 95 percent confidence interval [CI], -0.31 to 0.08; pnoninferiority <0.0001), confirming noninferiority of IDeg vs IDet in the primary endpoint. [Lancet Diabetes Endocrinol 2023;11:86-95]
Post-hoc analyses of the EXPECT trial showed no between-group differences in any hypoglycaemia (estimated RR, 0.97; 95 percent CI, 0.74–1.27), nocturnal hypoglycaemia (estimated RR, 0.90; 95 percent CI, 0.60–1.33), severe hypoglycaemia (estimated RR, 1.49; 95 percent CI, 0.23–9.80), and maternal adverse events (estimated RR, 1.17; 95 percent CI, 0.89–1.54). No perinatal or neonatal deaths were reported in the study.
Practical tips on IDeg use
“For patients with T2DM, IDeg can be initiated at 0.2 U/kg at any time of the day based on patients’ preference, to enhance adherence. The IDeg dose should be titrated until fasting glucose is within target range. Dose adjustment or discontinuation of other concomitant OADs, especially sulfonylurea, may be necessary,” Lock advised.
“When switching from basal insulin BID to once-daily IDeg, we may need to reduce the total daily basal insulin dose by 10–20 percent, followed by dose titration,” Lock added.
Summary
IDeg is a once-daily, ultra-long-acting basal insulin with stable glucose lowering effect and minimal risk of hypoglycaemia. With long duration of action, IDeg allows flexibility in timing of drug administration. Both clinical trials and real-world evidence support IDeg use in patients with T1DM or T2DM.