Atezolizumab + bevacizumab tops sorafenib in unresectable HCC




The combination of atezolizumab and bevacizumab (atezo-bev) delivered better overall survival (OS) and progression-free survival (PFS) outcomes than sorafenib in patients with untreated, locally advanced metastatic or unresectable hepatocellular carcinoma (HCC), the phase III IMbrave150 trial has shown.
“Although early-stage [HCC] may be curable by resection, liver transplantation, or ablation, most patients present with unresectable disease and have a poor prognosis,” said the researchers. Moreover, the approved first-line treatments* are tied to significant side effects that impair quality of life (QoL), hence the need for alternatives. [N Engl J Med 2008;359:378-390; Lancet 2018;391:1163-1173]
Primary analysis results showed a hazard ratio (HR) for death of 0.58 in favour of atezo-bev (p<0.001). [ESMO Asia 2019, abstract LBA3]
At 12 months, estimated OS rate was longer with atezo-bev vs sorafenib (67 percent vs 55 percent), as was PFS (median, 6.8 vs 4.3 months; HR, 0.59; p<0.001). [N Engl J Med 2020;382:1894-1905]
“The early separation of the Kaplan–Meier curves for OS was maintained over time despite a higher proportion of [sorafenib recipients] receiving subsequent systemic therapy, including immunotherapy,” the researchers explained. Despite the inclusion of a high-risk subgroup usually excluded in trials (ie, macrovascular invasion), favourable efficacy was still achieved, they added.
Compared with sorafenib-treated patients, atezo-bev recipients had higher objective response rates (ORR; 27 percent vs 12 percent [RECIST] and 33 percent vs 13 percent [HCC-specific mRECIST**]; p<0.001 for both) and disease control rate (74 percent vs 55 percent). Complete response was observed in 18 atezo-bev recipients as opposed to none with sorafenib.
Atezo-bev use led to longer median time to deterioration of QoL (11.2 months vs 3.6 months; HR, 0.63) and physical (13.1 months vs 4.9 months; HR, 0.53) and role functioning (9.1 months vs 3.6 months; HR, 0.62) vs sorafenib. The researchers noted that the rates in the atezo-bev arm were markedly longer than the median PFS – an effect that was not seen with sorafenib.
Taken together, the 42-percent lower hazard of death and longer OS with atezo-bev are reinforced by a 2.5-month increase in median PFS, a corresponding 41-percent drop in the hazard of disease progression or death, and a 27-percent ORR, noted the researchers.
Tolerable combination
Higher rates of serious adverse events (AEs; 38 percent vs 31 percent) and discontinuation due to AEs (16 percent vs 10 percent) were observed with atezo-bev vs sorafenib. Fifteen percent of atezo-bev recipients had grade 3/4 hypertension, which according to the researchers, is consistent with the known safety profile of bevacizumab. Nonetheless, there were no new or unexpected toxic effects reported.
Gastrointestinal (GI) disorders were the most common causes for atezo-bev withdrawal; however, this is expected in patients with cirrhosis and liver cancer, noted the researchers. “Bleeding … is a known adverse reaction to bevacizumab, and upper GI bleeding is a common and life-threatening complication,” they added. Nonetheless, upper GI bleeding rate with atezo-bev was only 7 percent.
Biomarker analyses
The study included 501 patients who were randomized 2:1 to receive IV atezolizumab 1,200 mg plus IV bevacizumab 15 mg/kg Q3W, or oral sorafenib 400 mg BID. The assigned regimens were given until unacceptable toxicity or loss of clinical benefit occurred.
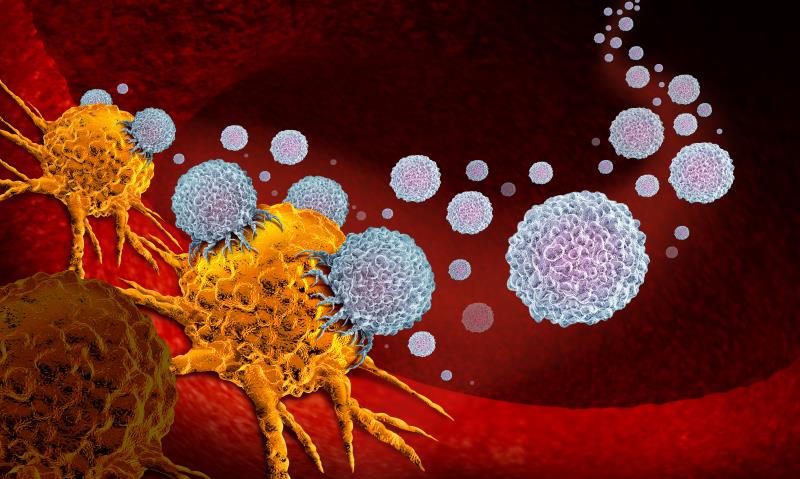
Bevacizumab targets VEGF*** while atezolizumab selectively targets PD-L1. [Liver Int 2009;29:284-290; Nature 2014;515:563-567] “Anti-VEGF therapies … may enhance anti–PD-1 and anti–PD-L1 efficacy by reversing VEGF-mediated immunosuppression and promoting T-cell infiltration in tumours,” noted the researchers.
“[Collectively, the efficacy findings were] generally consistent across clinical subgroups and confirms [evidence reflecting] the clinical benefit of targeting both angiogenesis and PD-L1 signalling in unresectable liver cancer,” said the researchers.
Despite the association between PD-L1 positivity and longer PFS in patients with untreated metastatic renal cell carcinoma receiving atezo-bev, [Lancet 2019;393:2404-2415] the predictive value of PD-L1 status for the efficacy of PD-1 and PD-L1 inhibitors or combination therapies in HCC remains unclear, noted the researchers. Tissue or blood biomarker analyses are thus warranted to identify biomarkers of response, as well as patients who would benefit most from the atezo-bev combination regimen.