A prospective study has shown the potential of a new algorithm – the FibroScan-AST (FAST) score – to identify patients with nonalcoholic steatohepatitis (NASH) with significant activity and fibrosis.
Nonalcoholic fatty liver disease (NAFLD) is now the most common cause of chronic liver disease (CLD) globally and is one of the main indications for liver transplants in Europe and the US. [Nat Rev Gastroenterol Hepatol 2018;15:11-20; J Hepatol 2019;71:313-322; Gastroenterology 2011;141:1249-1253] While most do not progress to advanced fibrosis or cirrhosis, the high prevalence of NAFLD highlights the potential to develop CLD. “A key challenge is the identification of patients who are at greatest risk of clinical progression [to] fibrosis and who might benefit from treatment with new pharmacotherapies,” said the researchers.
“[Our findings showed that] the FAST score provides an efficient way to noninvasively identify patients at risk of progressive NASH for clinical trials or [emerging pharmacotherapies] and thereby reduce unnecessary liver biopsy in patients unlikely to have significant disease,” they added.
The analysis included a derivation cohort (n=350), which is a cross-sectional, multicentre study conducted prior to validation in external validation cohorts* (n=1,026). Consecutive patients attending tertiary liver clinics in UK aged ≥18 years scheduled to have liver biopsy for investigation of suspected NAFLD were included in the derivation cohort. [Lancet Gastroenterol Hepatol 2020;5:362-373]
Predictive performance of FAST score in terms of discrimination, calibration, and diagnostic accuracy indicated an AUROC** of 0.80, with satisfactory calibration of predicted probabilities. This was similar to the AUROCs in the bootstrap sample and the original data (0.803 and 0.804, respectively).
External validation cohorts revealed similar AUROCs ranging from 0.80 to 0.95, with good to excellent discrimination in all except for the Turkish NAFLD cohort (AUROC of 0.74), which had modest performance. The best discrimination (AUROC of 0.95) was observed in the French bariatric surgery cohort.
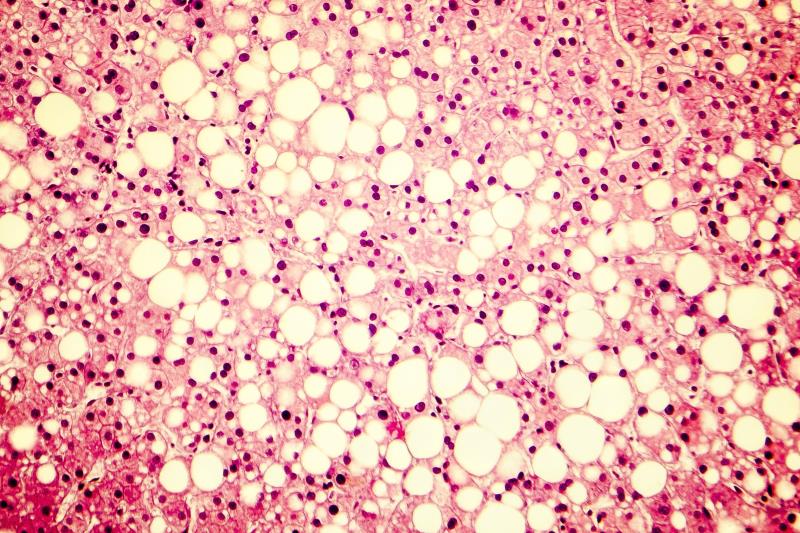
NASH: Driver of fibrosis in NAFLD
The presence of NASH and more profound liver injury are crucial drivers of fibrosis development in NAFLD, hence its importance in risk stratification. [Hepatology 2005;41:1313-1321] However, the currently used noninvasive markers to identify patients with active NASH and significant fibrosis cannot determine the presence or degree of inflammation, the researchers pointed out.
Therefore, the team aimed to develop an algorithm that could diagnose NASH in individuals with suspected NAFLD, significant liver fibrosis, and elevated NAFLD activity score. “This combination of criteria is important, as the presence of fibrosis alone is insufficient for recruitment to clinical trials,” they said.
“Moreover, the presence of inflammation defined by NASH and elevated NAS*** will be important in identifying patients who could benefit from anti-inflammatory therapies, as these interventions might not be as relevant for patients with fibrosis but [with minimal or without] inflammatory injury,” they added.
The noninvasive nature, low cost, and modest requirement for technical proficiency imply that the FAST score can be easily rolled out across clinical practices, said the researchers. “Roll-out is further aided by the free availability of the equation, which is also accessible through an app.”
However, despite the extensive validation with good performance across large global cohorts and wide availability of FibroScan devices, the target population appears to be an issue, pointed out the researchers. “[S]ome contend that … more advanced fibrosis (stage ≥3) should be the priority. At this stage, clinical trials are aiming to recruit patients with stage 2 and 3 fibrosis … [We] believe that stage ≥2 fibrosis constitutes a reasonable target group.”
Overall, the FAST score may assist clinicians and investigators in making informed decisions and streamline the need for liver biopsies among patients with NASH in clinical care, said the researchers. Further exploration is warranted to evaluate FAST score performance in primary care.