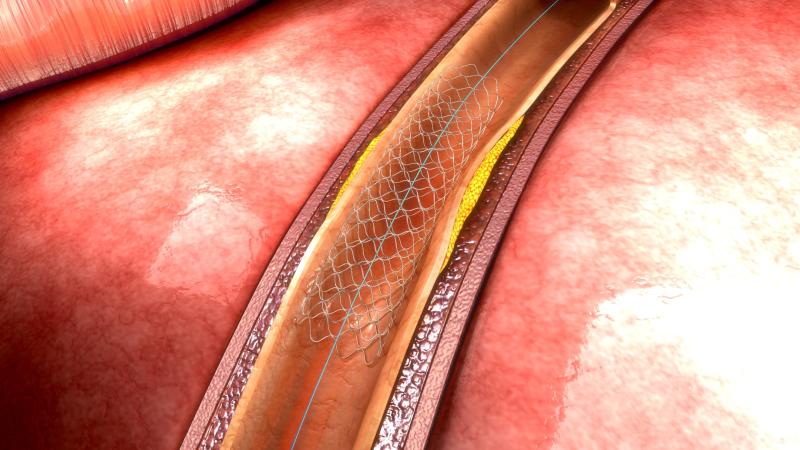
Long-term treatment with more potent antithrombotic therapy lowers spontaneous atherothrombotic events and prevents complications related to stenting of the culprit lesion following acute coronary syndrome (ACS), suggests a recent study.
“In patients undergoing percutaneous coronary intervention [PCI] for ACS, spontaneous events predominate after 30 days, with the later-phase cardiovascular benefit of potent dual antiplatelet therapy driven largely by reducing de novo atherothrombotic ischaemic events,” the researchers said.
Of the patients included in the TRITON-TMI 38* study, which randomized participants to prasugrel or clopidogrel, 12,844 with ACS received at least one stent. Myocardial infarction (MI) and cardiovascular death were categorized as follows: procedural (related to revascularization); definite or probable stent thrombosis (ST); or spontaneous (non-ST or nonprocedural-related). Median follow-up was 14.5 months.
Of the first events that occurred within 30 days, 584 (69.0 percent) were procedural, 126 (14.9 percent) ST-related and 136 (16.1 percent) spontaneous. After 30 days, 22 (4.7 percent) events were procedural, 63 (13.5 percent) ST-related and 383 (81.8 percent) spontaneous.
Treatment with prasugrel significantly reduced the incidence of MI or cardiovascular death for ST-related (1.0 percent vs 2.1 percent; p<0.001) and spontaneous events (3.9 percent vs 4.8 percent; p=0.012), with a directionally consistent numerical reduction in procedural events (4.4 percent vs 5.1 percent; p=0.078). However, prasugrel led to more spontaneous, but not procedural, major bleeding.
“Recent emphasis on reduced duration and/or intensity of antiplatelet therapy following PCI irrespective of indication for PCI may fail to account for the substantial risk of subsequent nontarget lesion events in ACS patients,” the researchers said.
*Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition With Prasugrel–Thrombolysis In Myocardial Infarction 38