Use of a semi-automated surgical robot for pedicle screw placement is feasible and boasts of a high technical and clinical accuracy, as shown in a cadaver study.
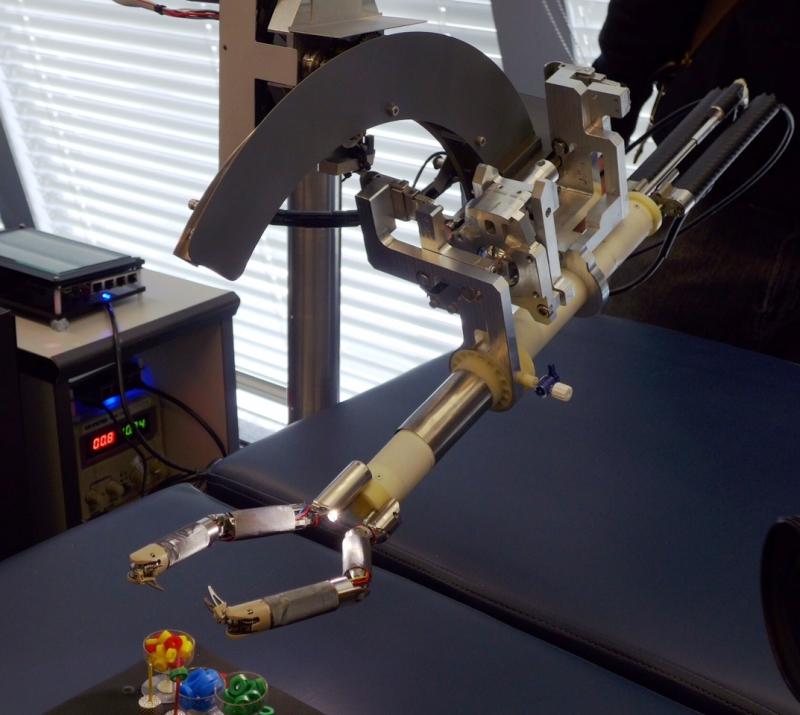
To assess the feasibility, accuracy and efficacy of a new robotic guidance system, a custom robotic arm was integrated into a hybrid operating room (OR) equipped with an augmented reality surgical navigation system (ARSN).
The robot mounted on the OR table was used to assist in placing Jamshidi needles in 113 pedicles in four cadavers, while the ARSN system helped in planning screw paths and directing the robot. The robot arm autonomously aligned with the planned screw trajectory, then the surgeon inserted the Jamshidi needle into the pedicle.
Accuracy was measured via verification cone beam computed tomography images with the planned paths superimposed. Pedicle screw diameters were then simulated on the placed Jamshidi needles to provide a clinical grading according to the Gertzbein scale.
The novel robot-guided system achieved a technical accuracy at bone entry point of 0.48±044 mm in the axial plane and 0.68±0.58 mm in the sagittal plane, with angular errors of 0.94±0.83° and 0.87±0.82°, respectively. [Sci Rep 2020;10:7522]
The mean navigation time from skin incision to placed Jamshidi needle following a planned path was 96±37 seconds. No statistically significant differences were seen between consecutive cadavers (pall>0.05). The time to reposition the robot (every five levels) was 106±71 seconds.
A statistically superior accuracy was seen with the robotic guidance system (p<0.001) as compared with ARSN without robotic assistance. Notably, the simulated pedicle screw grading resulted in 100-percent clinical accuracy.
In recent meta-analyses, robotic guidance demonstrated reliable but not superior clinical accuracy when compared to pedicle screw placement with standard fluoroscopic guidance. [Spine (Phila Pa 1976) 2018;43:1670-1677; Int J Comput Assist Radiol Surg 2016;11:2273-2281; World Neurosurg 2018;116:433-443.e438]
In contrast, another meta-analysis reported lower rates of accuracy among navigation and robot-guided surgeries than freehand surgeries. [World Neurosurg 2018;116:433-443.e438]
“This highlights the complexity of choosing a good outcome parameter for robot-guided surgery and the possible shortcomings of clinical grading scales alone,” the researchers said.
“Therefore, it is our belief that there is an added benefit in reporting all available accuracy data and not solely rely on either clinical grading scales or absolute, technical accuracies for new technologies, when outcome data such as revision rates or complication rates are not available,” they added.
In addition, a key issue in accurate pedicle screw placement as shown in previous studies was the correct approach and entry into the pedicle, which is partly determined by a “well-chosen bone entry point, devoid of ridges and slopes, which may deflect the instrument used to penetrate the bone.” [Spine (Phila Pa 1976) 2019;44:1097-1104; Neurosurg Focus 2014;doi:10.3171/2014.1.FOCUS13516; Medicine (Baltimore) 2016;95:e4834; PLoS One 2016;11:e0153235]
“Surgical navigation with 3D representation of the deep bone anatomy adequately addresses the identification of a good bone entry point and the augmented reality visualization is especially helpful in this respect,” the researchers noted. [Spine (Phila Pa 1976) 2019;44:1097-1104]
The current study was limited by its small sample size, lack of a control group and that no actual pedicle screws were placed.