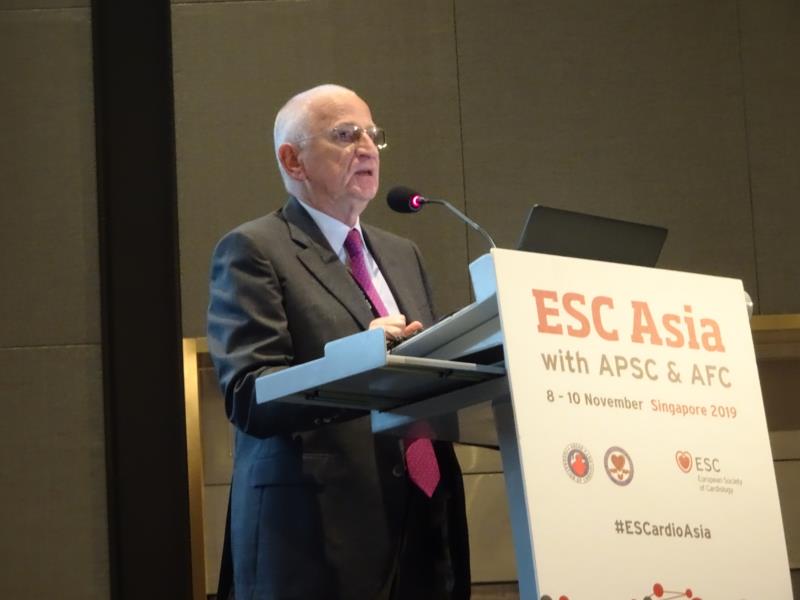
Treatment options for patients with heart failure with preserved ejection fraction (HFpEF) remain limited, with benefits that are marginal at best, according to Prof Michel Komajda, past president of the European Society of Cardiology (ESC), at their recently concluded 2019 Asia Congress (ESC Asia 2019).
Citing the 2016 ESC Guidelines, Komajda pointed out that “no treatment has yet been shown convincingly to reduce morbidity and mortality in patients with HFpEF or midrange ejection fraction.”
Indeed, in the same document, the ESC identifies just two recommendations for HFpEF. First, patients should be screened for cardiovascular or noncardiovascular comorbidities, which should then be managed accordingly. Then, in the case of congested patients, diuretics may be used to help relieve symptoms.
The list of treatment recommendations has since expanded a bit, especially for stage C HFpEF, but overall, options remain restricted.
“Why are the recommendations so limited? Because when look[ing] at the large outcome trials that have been performed in HFpEF, it is quite depressing,” Komajda continued. The TOPCAT cohort, for instance, found no clear benefit of spironolactone over placebo in terms of the primary composite outcome of cardiovascular death, heart failure hospitalization or resuscitated cardiac arrest.
Other trials have revealed similarly null effects of different therapeutic agents such as candesartan, irbesartan and perindopril.
In the PARAMOUNT proof-of-concept study, however, the combination of sacubitril and valsartan resulted in significant clinical benefit over valsartan alone, particularly on left atrial volume and the concentrations of N-terminal pro B-type natriuretic peptide. This led to the PARAGON-HF study, which sought to compare the two treatment regimens in a randomized, double-blind trial.
PARAGON-HF confirmed the relative advantage of the combination treatment in terms of different efficacy endpoint: the composite of total HF hospitalizations and cardiovascular death, and its individual components.
However, subgroup analyses found important moderating effects of sex and left ventricular ejection fraction. In particular, sacubitril-valsartan therapy was only significantly effective in females and in patients who fell below the median ejection fraction threshold of 57 percent. The value of the intervention failed to reach statistical significance otherwise.
“Once again, the trial is not convincingly positive, but rather neutral in HFpEF,” said Komajda.
“And so, what remain is a lot of question marks regarding the current treatment of HFpEF particularly on important endpoints, such as hospitalization for heart failure or mortality in all forms or cardiovascular mortality,” he added. “One of the challenges we are facing is that we have not so far found the proper window of opportunity between patients who are too well to benefit and those who are too sick to benefit.”