Antithrombotics in COVID-19: Guidance in times of uncertainty




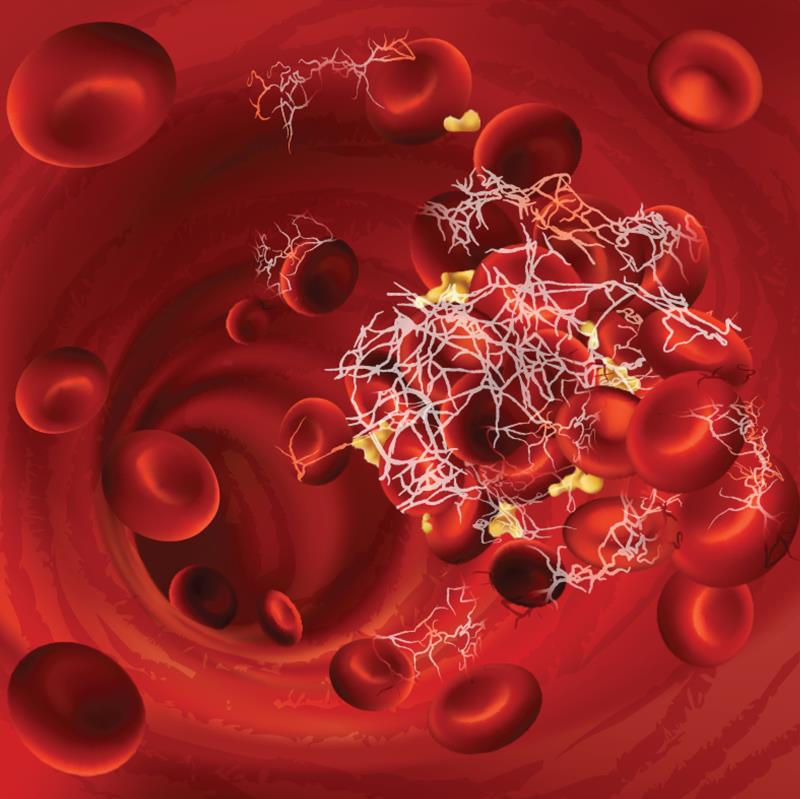
As the world learns more and more about the enigmatic nature of the pandemic that is COVID-19, emerging evidence shows that erratic blood clotting — or coagulopathy — often complicates severe COVID-19 cases.
Given the urgency of the situation and the widely varying practice in handling the matter, the 36-person Global COVID-19 Thrombosis Collaborative Group (hereafter referred to as JACC guidance) has compiled a guidance review — endorsed by various professional societies* including the ISTH— to provide practical guidance to clinicians at the frontline. [J Am Coll Cardiol 2020;75:2950-2973]
Following this, expert panel from CHEST** has also released a set of 22-statement guidelines echoing largely similar principles in managing thrombotic disease in COVID-19 patients. [Chest 2020;doi:10.1016/j.chest.2020.05.559]
“The guidance statements were specifically created to address what were felt to be common, urgent clinical questions that frontline providers are likely to face regarding VTE*** and hypercoagulability in patients with COVID-19,” said the CHEST expert panel.
“Very little evidence exists in the COVID-19 population. The panel thus used expert consensus and existing evidence-based guidelines to craft the guidance statements,” they added.
One overarching theme of both guidelines revolves around how to diagnose and manage thrombotic disease in COVID-19 patients. In addition, the Thrombosis Collaborative Group also discussed on the management of patients without COVID-19 who have thrombotic disease, and highlighted the potential drug-drug interactions between investigational treatments for COVID-19 and antithrombotic medications.
Lethal signs
As experts observed, the coagulopathy found in most severe COVID-19 patients often manifests as disseminated intravascular coagulation (DIC) — a prothrombotic state which predisposes patients to VTE.
DIC itself is a strong predictor of mortality: 71 percent of COVID-19 patients who died in a hospital in Wuhan, China had ISTH-defined DIC compared with only 0.6 percent among those who survived. [J Thromb Haemost 2020;18:844-847]
One consistent finding associated with coagulopathy in hospitalized patients with COVID-19 is elevated D-dimer levels, a degradation product of crosslinked fibrin. Along with increased fibrinogen levels, these abnormalities often parallel the rise in inflammatory biomarkers such as C-reactive protein.
Routine ultrasound screening for asymptomatic deep vein thrombosis in hospitalized patients with moderate or severe COVID-19 who presented with elevated D-dimer (>1,500 ng/mL) is currently discouraged due to positioning, a view iterated in both JACC and CHEST guidelines.
Unlike the classic coagulopathy generally seen with other severe infections, prolongation of PT and/or aPTT# was mild in COVID-19 patients and thrombocytopenia is uncommon at admission. [https://www.hematology.org/covid-19/covid-19-and-coagulopathy. Accessed 22 Jun 2020]
Antithrombotics: What and how much to give?
Due to a heightened risk of abnormal clotting, the CHEST guidelines called for routine anticoagulant thromboprophylaxis in all hospitalized patient with COVID-19, unless contraindicated.
Along the same vein, the JACC guidance recommended that prophylactic doses of anticoagulation be given to prevent VTE in hospitalized patients with moderate or severe COVID-19 and without overt bleeding, regardless of the presence of DIC.
The JACC guidance further added that hospitalized COVID-19 patients without DIC should undergo risk stratification for VTE prophylaxis. For patients in whom pharmacological prophylaxis is contraindicated, the experts considered intermittent pneumatic compression a reasonable alternative, especially in immobilized patients.
While the JACC experts said “The choice of agents and dosing should be based on available guideline recommendations,” they also noted that prophylactic low-molecular-weight heparins (LMWHs) or subcutaneous unfractionated heparin (UFH) are recommended in the WHO interim guidance.
“Once-daily dosing regimen of LMWHs may be advantageous over [twice-daily] UFH to reduce personal protective equipment [PPE] use and exposure of healthcare workers,” they explained.
A major question regarding prophylactic anticoagulation remains: what is the appropriate dosing (standard, intermediate, or escalated) for COVID-19 patients?
Based on the CHEST guidelines, the current standard dose is recommended over intermediate (increased weight-based dosing or twice-daily LMWH) or full-on therapeutic dose, as per existing guidelines, for both acutely or critically ill hospitalized patients with COVID-19.
The same sentiment was echoed by the JACC experts. “For hospitalized patients with COVID-19 [regardless of DIC], there are insufficient data to consider routine therapeutic or intermediate-dose parenteral anticoagulation with UFH or LMWH.”
How about oral anticoagulants and antiplatelets?
While LMWH is preferred over UFH for thromboprophylaxis in general, both LMWH and UFH are favoured when compared with a direct oral anticoagulant (DOAC) in acutely or critically ill patients, according to the CHEST guidelines.
“In critically ill or acutely ill hospitalized patients with COVID-19, we recommend against the use of antiplatelet agents for VTE prevention,” wrote the CHEST panel experts.
In addition, there is no known association between the use of antithrombotic agents and risk of developing severe COVID-19. “If patients have been taking antithrombotic agents for prior known thrombotic disease, they should continue their antithrombotic agents as recommended,” urged the JACC expert panel. The advice applies to outpatients with mild COVID-19 as well as patients without COVID-19.
However, the JACC experts also pointed out that antiplatelet agents and oral anticoagulants can potentially interact with investigational COVID-19 therapies. For instance, lopinavir/ritonavir inhibits CYP3A4 metabolism, which may lead to enhanced effects of ticagrelor but reduced efficacy of clopidogrel. “Therefore, the concomitant use of these agents along with lopinavir/ritonavir should be cautioned.”
Beyond hospital setting
For outpatients with mild COVID-19, the JACC experts do not recommend indiscriminate use of pharmacological VTE prophylaxis but encourage mobility (physical activity) and assessment for VTE and bleeding risk in these patients. Those with elevated VTE risk and not at high bleeding risk can be considered for pharmacologic prophylaxis on an individual case basis.
For hospitalized COVID-19 patients who have been discharged, the expert panel considers routine screening for VTE risk a reasonable approach to decide on the use of post-hospital pharmacological prophylaxis for up to 45 days after discharge.
Looking forward
“Clearly, we still need well designed randomized trials to answer many of our pressing questions. These include optimal dosing of prophylactic anticoagulant therapy, patients who might benefit from full dose anticoagulant treatment, and the unique role of macro and microthombosis in COVID-19,” the CHEST expert panel pointed out.
“[We] consider this to be a living document … [and] look forward to updating this guidance when well-designed trials have been completed,” they stated.