COVID-19 may be linked to liver dysfunction, HBV reactivation




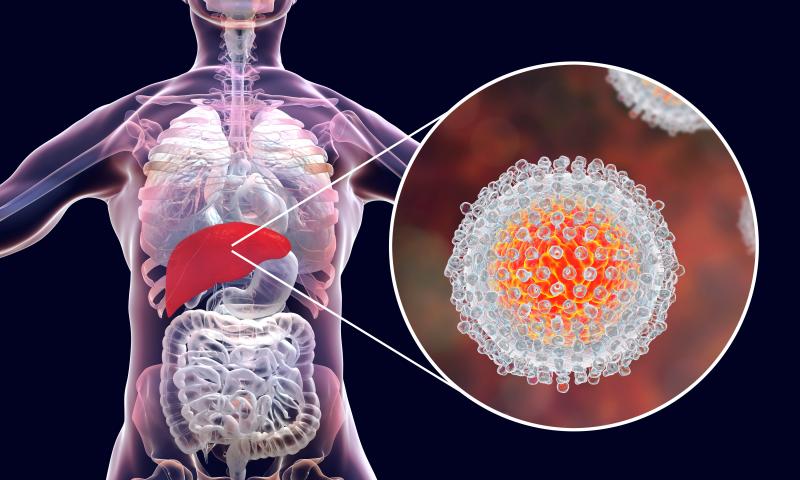
Liver dysfunction may also be a manifestation of the coronavirus disease 2019 (COVID-19), according to a new study. In patients with chronic hepatitis B virus (HBV) infection, COVID-19 may also trigger reactivation of the virus.
“More evidence is urgently needed to guide the screening of HBV coinfection and management of comorbidity of CHB during the pandemic of COVID-19,” researchers said.
The retrospective study included 347 COVID-19 patients, of whom 21 had chronic HBV infection upon enrollment. Propensity score matching resulted in 20 HBV patients matched to 51 non-HBV comparators. By the end of follow-up, all 71 participants in the final cohort saw clearance of the SARS-CoV-2 virus. [Hepatol Res 2020;10.1111/hepr.13553]
The median time to virus clearance was 21 days in the HBV group. This was longer than in the non-HBV comparators (median, 14 days), although the researchers reported no between-group significant difference in the likelihood of clearing SARS-CoV-2 over time (p=0.1). No deaths were recorded.
Similarly, the probability of developing severe COVID-19 was comparable between groups, with 30 percent and 31.4 percent of the HBV and non-HBV patients, respectively, experiencing such disease progression (p=0.97). This was confirmed through multivariate analysis (adjusted hazard ratio, 1.39, 95 percent confidence interval, 0.43–4.59; p=0.58).
Liver dysfunction was also relatively common in both HBV and non-HBV groups. At least once during hospitalization, abnormal measurements of alanine aminotransferase (ALT) were reported in 35 percent and 37.25 percent of the respective groups (p=0.86). A similar pattern was reported for concentrations of aspartate aminotransferase (AST), which showed abnormal levels in 30 percent and 31.37 percent of the patients, respectively (p=0.91).
Abnormal measurements of gamma-glutamyl transferase (40 percent and 37.2 percent, respectively; p=0.83) and total bilirubin (45 percent and 39.22 percent, respectively; p=0.91) at least once during hospitalization were also common in both patient groups.
Notably, the researchers saw that COVID-19 may also trigger HBV reactivation. Of the 20 HBV patients, 19 had HBV DNA viral load testing at least twice while admitted. Of these, 15 had consistently low or undetectable levels, two showed consistently high levels, and three experienced HBV reactivation.
In two of the reactivation cases, the researchers hypothesized that methylprednisolone medication may have had a role to play.
“However, one of the three patients who did not receive any corticosteroid also developed hepatitis B reactivation,” they said. “Our results suggested that for COVID-19 patients who had chronic HBV infection, whether or not corticosteroids were used, they could have a risk of hepatitis B reactivation.”
“The results in this study imply that it is necessary to monitor the liver function of COVID-19 patients, as well as the HBV DNA levels for those with HBV during the whole disease course,” they added.