Is ticagrelor protective against osteoarthritis too?




Ticagrelor reduces the risk of developing osteoarthritis (OA) by about 30 percent compared with another antiplatelet, clopidogrel, as shown in a recent study.
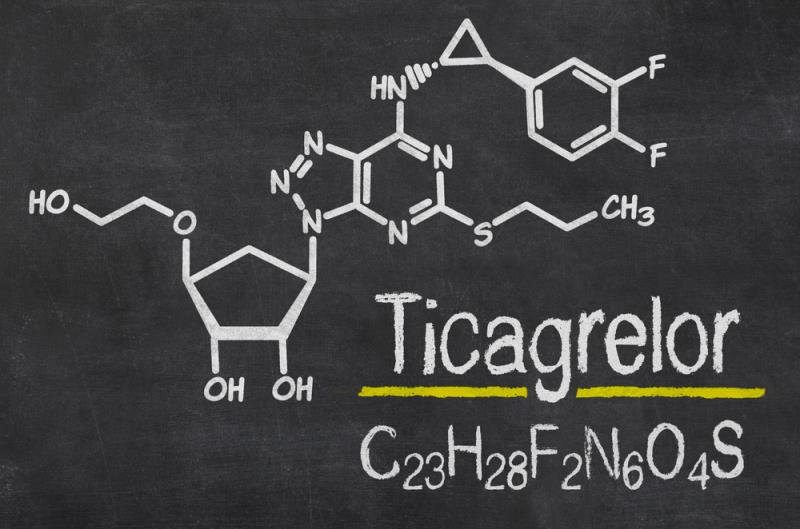
Used to treat patients with coronary artery disease, the two antiplatelet drugs “both work by antagonizing the binding of adenosine diphosphate to the P2Y12 receptor on platelets, thereby reducing platelet aggregation,” according to researchers.
“We postulate that the potential underlying biologic mechanism explaining these findings is an increase in extracellular adenosine caused by ticagrelor, which does not occur with clopidogrel,” they added.
The analysis included a propensity-score matched cohort of 7,007 ticagrelor‐treated and 14,014 clopidogrel‐treated patients, with a median number of 287 and 284 days on treatment, respectively. The median age of the entire population was 64 years, and 73 percent of the patients were male.
Over 5 years of follow-up, there were fewer patients who developed OA in the ticagrelor group (7.6 percent vs 10.2 percent). The incidence rate was 62.8 per 1,000 person years, compared to 89.2 per 1,000 person years in the clopidogrel group. [Arthritis Rheumatol 2020;doi:10.1002/art.41412]
On multivariate Cox regression analysis, ticagrelor was associated with a 29-percent lower risk of incident OA (hazard ratio [HR], 0.71, 95 percent confidence interval [CI], 0.64–0.79; p<0.001). This risk-reduction benefit was observed for OA of the hands (HR, 0.71, 95 percent CI, 0.53–0.96; p=0.025) and knees (HR, 0.769, 95 percent CI, 0.58–0.83; p<0.001) but not hips (HR, 0.72, 95 percent CI, 0.34–1.53; p=0.394).
The number of patients who underwent hip or knee arthroplasty was small in both groups (23 with ticagrelor vs 49 with clopidogrel), and there was no difference observed in the risk of joint arthroplasty (HR, 0.90, 95 percent CI, 0.55–1.49; p=0.690).
“We believe that even [a] relatively short treatment period [of around 287 days with ticagrelor] may provide protection against developing OA over the subsequent years. It is not clear how long this effect may last, as the follow-up period for this study ended at 5 years, with a relatively small number of patients at risk after 3 years,” the researchers said.
Ticagrelor increases extracellular adenosine concentration by suppressing the nucleoside transporter ENT1, which prevents intracellular uptake of adenosine. In animal models, extracellular adenosine has been shown to reduce inflammatory responses and ameliorate OA in mouse and rat models. [J Am Coll Cardiol 2014;63:2503-2509; Basic Clin Pharmacol Toxicol 2017;120:610-614; FASEB J 2016;30:3887-3900: Nat Commun 2017;8:15019; Sci Rep 2019;9:7430]
Likewise, a commonly used disease modifying antirheumatic drug (DMARD) for rheumatoid arthritis, methotrexate, reportedly exerts, to some extent, its anti-inflammatory effect by increasing extracellular adenosine. While there is minimal data evaluating this pathway in patients with OA, preliminary data from the Pain Reduction with Oral Methotrexate in knee Osteoarthritis (PROMOTE) trial indicate that methotrexate may improve OA symptoms as well. [Nat Rev Rheumatol 2016;12:731-742; Nat Rev Rheumatol 2019;15:355-363]
“These findings suggest that extracellular adenosine may play an important role in reducing cartilage inflammation and damage, and that it might serve as a therapeutic target for preventing and treating OA in humans,” they stated.
“Ticagrelor carries a risk of bleeding due to its antiplatelet effects, and thus we hope that data from this study will inform future research to identify safer therapies for OA that can similarly increase extracellular adenosine,” they added.