
Oral H1-antihistamines are the initial treatment of choice for allergic rhinitis (AR) and chronic urticaria in the primary care setting. However, in a diverse population of patients with AR and urticaria, primary care physicians are faced with the challenge of prescribing the best therapy amid a wide armamentarium of antihistamines available.
Although international guidelines for allergy are in place, there is a clear gap between guidelines and real-world practice. Current guidelines do not provide sufficient stepwise approach targeted to primary care, and often do not address the maximum duration of antihistamine use, what to do in the event of a symptom rebound following treatment, and which antihistamines to use in special populations, for example, in paediatric and elderly patients.
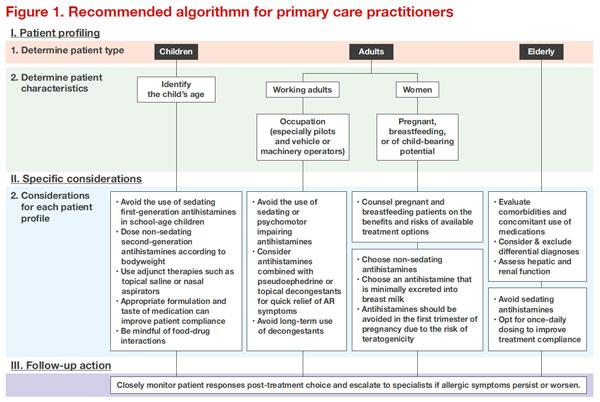
Given these gaps in guidance for primary care, experts from relevant specialties – allergology, paediatrics, otorhinolaryngology, and dermatology – in Malaysia came out with a consensus and recommendations to guide antihistamine choice for AR and chronic spontaneous urticaria (CSU). This entails patient profiling to identify patient needs, type and characteristics, considerations for each patient profile, and monitoring of treatment response, as well as referral to a specialist when required [Figure 1]. [Ther Clin Risk Manag 2019;15:1267-1275]
In school-age children where the impact of sedation on learning ability is a great concern, the authors recommend second-generation antihistamines. Loratadine (Clarityne®, Bayer), is a nonsedating second-generation antihistamine with proven efficacy in AR. In one study, loratadine significantly reduced sneezing, rhinorrhoea, and nasal itching in children aged 3–12 years. [Asian Pac J Allergy Immunol 2001;19:171-175] Loratadine also minimized allergy-induced learning impairments vs diphenhydramine in children with seasonal AR. [Ann Allergy 1993;71:121-126]
Taste-masking of bitter drugs in liquid formulations can also improve treatment compliance and outcome in children. As parents commonly mix medication with food or beverages to enhance taste, understanding the compatibility of medicine formats with food and beverages is important, said the authors. This is because certain antihistamines (eg, fexofenadine and bilastine) interact with grapefruit juice or any acidic fruit juice, decreasing the drug’s bioavailability.
Furthermore, night-time dosing of sedating antihistamines, as is the common practice to aid sleep, should be avoided. Evidence showed that use of night-time antihistamine with a morning dose of a nonsedating antihistamine only increased somnolence at daytime and was no better than a nonsedating antihistamine alone at providing superior relief of CSU symptoms. [Br J Dermatol 2014;171:148-154] Moreover, some second-generation antihistamines (eg, cetirizine, levocetirizine) may still induce sedation-like effects, despite being selective for peripheral H1-receptors.
As for women of child-bearing age (15–49 years), careful evaluation of the benefits vs risks should be done when prescribing antihistamines during pregnancy and lactation. Studies in animals have not shown any evidence of risk for loratadine and cetirizine; however, these medications should be used during pregnancy only if the benefit outweighs the risk to the foetus. Caution is also advised when prescribing second-generation antihistamines that affect psychomotor function.
In Asia where AR and CSU are more prevalent among the elderly, allergies may be viewed as less life-threatening than other major medical conditions, but symptoms such as nasal blockage and skin discomfort significantly compromise their quality of life. It is also reassuring to note that second-generation antihistamines (eg, loratadine, cetirizine) have demonstrated good cardiovascular safety in elderly patients. [Allergy Asthma Proc 2000;21:15-20] For patients with dementia, once-daily dosing is advised for convenience and better treatment compliance.
For all patient groups, referral to a specialist is advised when symptoms persist or worsen, or for difficult-to-treat cases. Long-term use of antihistamines requires a review of patient responses on a regular basis, said the authors. Currently, there is good safety data to support the use of second-generation antihistamines for up to 18 months.
Conclusion
Second-generation antihistamines are the recommended first-line treatment for mild AR and urticaria, with superior safety and improved efficacy compared to first-generation antihistamines. Patient profiling is an important tool that will help primary care physicians in the selection of antihistamines for different AR and CSU populations. Guidelines with specific recommendations pertinent to primary care are clearly warranted to improve management of AR and urticaria.