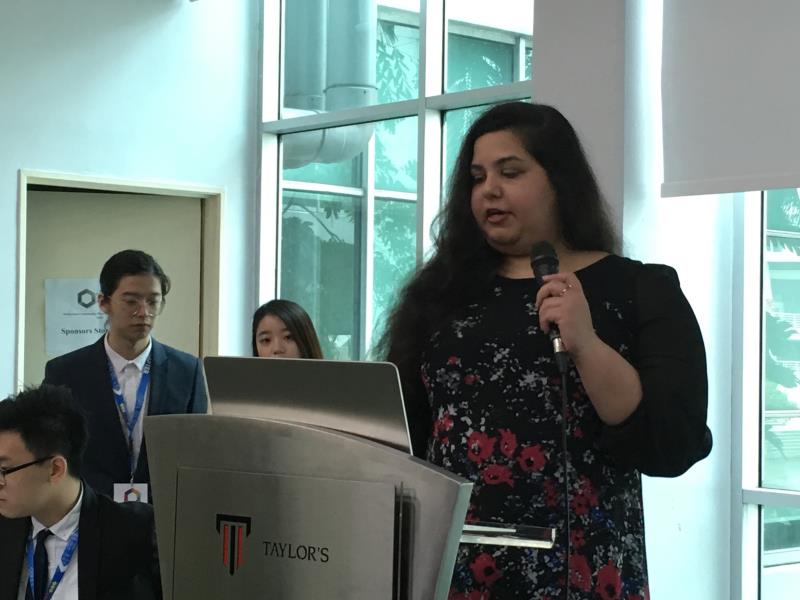
 Anisha Kaur Sandhu, clinical pharmacist and former member of the New Zealand Counties Manukau District Health Board.
Anisha Kaur Sandhu, clinical pharmacist and former member of the New Zealand Counties Manukau District Health Board.The extension of medication therapy adherence clinic (MTAC) services to community pharmacies could improve the delivery of Malaysian primary healthcare as it has in other countries, says an expert.
According to Anisha Kaur Sandhu, clinical pharmacist formerly of Middlemore Hospital, New Zealand, and a member of the Counties Manukau District Health Board, government support for the enhancement of pharmacist roles in New Zealand’s integrated healthcare framework has enabled the use of over 3,700 pharmacists to improve health coverage in an effective and flexible way.
“Pharmacists belong on the frontline of primary care in managing medication-related problems, reducing medication-related hospitalizations, being widely accessible, and providing direct patient-care services,” said Anisha, speaking at the recent Malaysian Community Pharmacy Business Forum 2019 (MyCBPF 2019) in Petaling Jaya.
New Zealand community pharmacies are entitled to offer a range of integrated pharmacist services including but not limited to long-term condition management, medicines therapy assessment, the Community Pharmacy Anticoagulation Monitoring Service (CPAMS), medicines use reviews (MUR), methadone maintenance treatment (MMT), oral contraceptive pill (OCP) dispensing, and flu vaccinations.
Describing the history of CPAMS implementation in New Zealand as an example, Anisha noted that the programme—which aimed to improve international normalized ratio (INR) point-of-care testing and warfarin dosage adjustment for patients with cardiovascular issues—was found to be a safe and effective service with significant improvements in time in therapeutic range (TTR) compared to usual care.
At present, MTACs in Malaysia are limited to public healthcare, with 13 types of MTAC services available in over 600 MOH facilities. Initiated in 2004, MTACs, especially for diabetes, have aimed to optimize drug therapies, improve adherence, and minimize adverse events.
A roadmap to local MTAC
Were community pharmacies to embrace MTAC, it would not only allow them to differentiate themselves from their peers—granting a competitive advantage—but it would expand the role and scope of community pharmacists, increasing recognition, and lifting the profile of the profession, said Anisha.
However, robust strategies would need to be put in place to cover the regulation and governance of services provided; training, accreditation and recertification processes; funding and payment structures; as well as guidelines and referral processes.
Anisha proposed a pared-down version of MTAC in community pharmacies which would be oriented more towards screening, counselling, and referrals, with a focus on providing specific services such as anticoagulant testing. To support its implementation, she suggested an official zoning system for various MTAC services with clear referral procedures to associated MOH clinics or prescribers in the public and private sectors.
“Developing technologies such as patient-friendly apps that could act as communication tools between community pharmacists and prescribers would also help create information sharing networks to support MTAC service provision at the community pharmacy level,” said Anisha.
She added that a strategic rollout of MTAC services nationwide through pilot projects would enable a thorough assessment of various renumeration and funding strategies, the level of education and training required for service provision, and patient perceptions towards the idea of the service.
“In terms of feasibility, one would need to consider what proportion of MTAC costs would be best shared by the government and community pharmacies, or covered by patients,” said Anisha.
Other challenges to surmount with regards to MTAC implementation in Malaysian community pharmacies included staffing inadequacies, change resistance, and poor pharmacist-prescriber relationships, she admitted.