Atrial fibrillation (AF) appears to be relatively common among patients with heart failure with reduced ejection fraction (HFrEF) and affects the prescription of guideline-recommended HF therapies, a recent study has shown.
The study included 8,253 patients (mean age, 72.3±11.8 years; 64.0 percent male) with chronic HFrEF. AF was detected using a 12-lead electrocardiogram and patient records were accessed for information on treatment regimens.
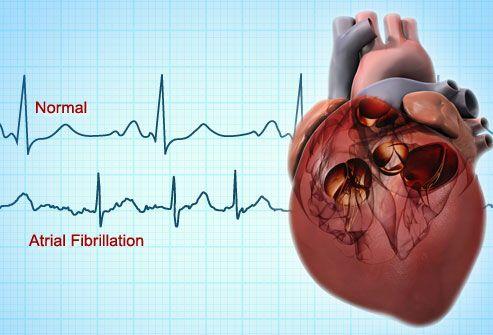
More than a quarter (25.6 percent; n=2,109) of the participants had AF based on ECG measurements during the most recent outpatient visit, or had a documented history of AF. These participants tended to be older than those without AF and were more likely to have more comorbidities.
In terms of treatment, AF participants were prescribed beta-blockers (81.7 percent vs 79.7 percent; p=0.04) and mineralocorticoid receptor antagonists (57.1 percent vs 51.7 percent; p<0.01) significantly more frequently than their non-AF counterparts. The same was true for diuretics (89.7 percent vs 80.6 percent; p<0.01), digoxin (40.1 percent vs 9.3 percent; p<0.01), oral anticoagulants (82.4 percent vs 41.7 percent; p<0.01) and non-vitamin K antagonist oral anticoagulants (7.3 percent vs 3.6 percent; p<0.01).
On the other hand, inhibitors of the renin-angiotensin system (76.1 percent vs 83.1 percent; p<0.01), amiodarone (12.9 percent vs 15.3 percent; p=0.04) and sotalol (2.7 percent vs 5.6 percent; p<0.01) were less commonly prescribed to AF patients.
“These results show the need for a better understanding of the efficacy and adherence of guideline-recommended HF therapy in patients with AF,” researchers said.