 In intermediate risk patients, the TAVR is found to have better outcomes
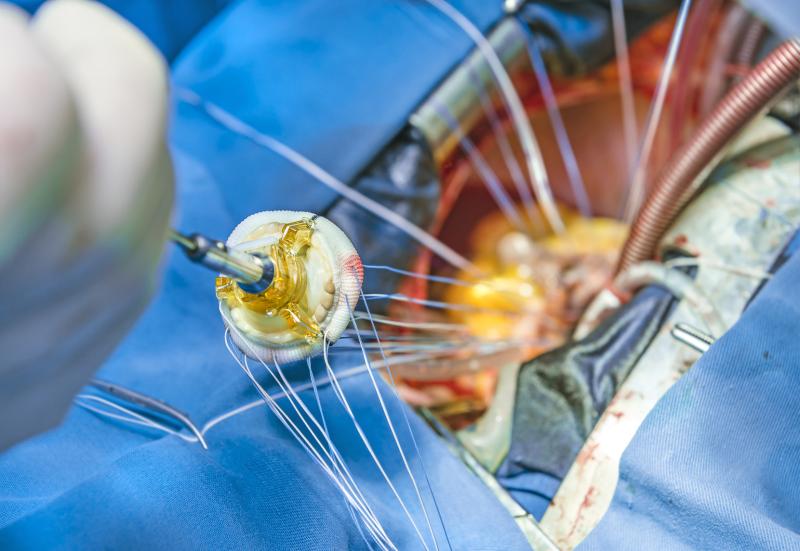
In intermediate risk patients, the TAVR is found to have better outcomesValve-in-valve (VIV) transcatheter aortic valve replacement (TAVR) leads to better short-term outcomes than redo surgical aortic valve replacement (SAVR) in patients treated for aortic bioprosthesis failure, a recent study has shown. During long-term follow-up, no difference is seen in major cardiovascular outcomes between the two treatment arms.
To assess the outcomes of VIV TAVR compared with redo SAVR, the investigators collected data on patients treated for aortic bioprosthesis failure using the French administrative hospital-discharge database between 2010 and 2019. Outcomes were analysed using propensity score matching.
Overall, 4,237 patients were identified in the database, of whom 717 were analysed in each treatment arm after matching for baseline characteristics. At 30 days, VIV TAVR resulted in lower rates of the composite of all-cause mortality, all-cause stroke, myocardial infarction, and major or life-threatening bleeding (odds ratio [OR], 0.62, 95 percent confidence interval [CI], 0.44–0.88; p=0.03).
No significant between-group difference was observed for the combined endpoint of cardiovascular death, all-cause stroke, myocardial infarction, or rehospitalization for heart failure (OR, 1.18, 95 percent CI, 0.99–1.41; p=0.26) during a median follow-up of 516 days.
However, patients in the VIV TAVR group were more frequently rehospitalized for heart failure and pacemaker implantation. Moreover, a time-dependent interaction was reported between all-cause and cardiovascular mortality following VIV TAVR (pinteraction<0.05).
“VIV TAVR and redo SAVR represent the two treatments for aortic bioprosthesis failure,” the investigators said. “Clinical comparison of both therapies remains limited by the number of patients analysed.”