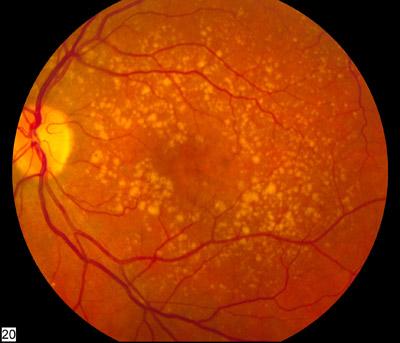
 The bright spots in this human eye scan are signs of macular degeneration. Photo credit: National Eye Institute
The bright spots in this human eye scan are signs of macular degeneration. Photo credit: National Eye InstituteThe combination of intravitreal aflibercept and antiplatelet-derived growth factor receptor β (anti-PDGFRβ) falls short of improving best-corrected visual acuity (BCVA) in patients with treatment-naïve neovascular age-related macular degeneration (nAMD), as compared with intravitreal aflibercept injection (IAI) monotherapy, a phase II study has shown.
Anatomic outcomes evaluating complete fluid resolution also favour IAI.
This study randomized 505 patients with nAMD 1:2:2 to low-dose combination intravitreal anti-PDGFRβ 1 mg and aflibercept 2 mg (LD combo), high-dose combination intravitreal anti-PDGFRβ 3 mg and aflibercept 2 mg (HD combo), or IAI alone every 4 weeks through week 12.
Patients in the HD combo and IAI groups were then rerandomized at week 12 to continue as assigned or switch from HD combo to IAI or IAI to HD combo and dosed every 4 weeks through week 28. During weeks 28 to 52, patients received treatment as needed per prespecified criteria.
Mean BCVA gains at week 12 from baseline were 5.8 letters with LD combo, 5.8 with HD combo and 7.5 with IAI (LD combo: p=0.21; HD combo vs IAI: p=0.01). The corresponding proportions of eyes that gained ≥15 letters were 12 percent, 19 percent and 22 percent.
Mean reductions in central retinal thickness from baseline were 126.1 μm with LD combo, 127.1 μm with HD combo and 126.9 μm with IAI. The proportions of eyes with complete resolution of fluid from baseline were 35 percent, 24 percent and 42 percent, respectively.
At week 28, vision and anatomic outcomes were consistent with those from week 12. Through week 52, the corresponding incidence of intraocular inflammation was 1.0 percent, 7.5 percent, 2.1 percent, 2.1 percent and 0 percent. The incidence of Anti-Platelet Trialists’ Collaboration–defined arterial thromboembolic events was 1.9 percent, 0.9 percent, 1.1 percent, 2.1 percent and 1.9 percent, respectively.
“Adverse events were consistent with the reported IAI safety profile, except for a higher frequency of intraocular inflammation in the HD combo group,” the authors said.