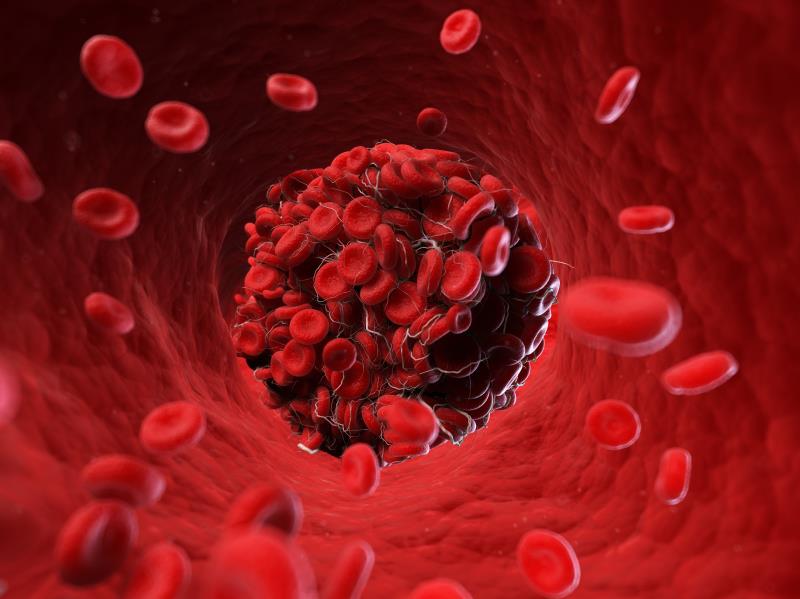
Patients with cancer who develop venous thromboembolism (VTE) could reduce their risk of VTE recurrence with the direct oral anticoagulant (DOAC) apixaban, which demonstrated noninferiority to subcutaneous dalteparin in the Caravaggio* trial.
“Our data show that apixaban is at least as effective as dalteparin – the current gold standard treatment – without any excess in major bleeding, which is a common concern when giving blood thinners,” noted study lead author Professor Giancarlo Agnelli from the University of Perugia, Perugia, Italy.
Participants in this multinational, open-label trial were 1,170 adults (mean age 67.2 years) with cancer** and newly diagnosed symptomatic or incidental acute proximal VTE (deep-vein thrombosis [DVT] or pulmonary embolism [PE]). Within 72 hours of VTE presentation, patients were randomized 1:1 to receive oral apixaban (10 mg BID for 7 days, followed by 5 mg BID) or subcutaneous dalteparin (200 IU/kg QD for 1 month, followed by 150 IU/kg QD) for 6 months. Median treatment duration was comparable between groups (178 and 175 days in the apixaban and dalteparin groups, respectively).
About 97 percent of patients had active cancer*** at baseline, with >60 percent undergoing treatment. Colorectal and lung cancer were the most common cancers in both apixaban (21.0 and 18.2 percent, respectively) and dalteparin (19.5 and 16.4 percent, respectively) recipients.
Over the study period, the incidence of recurrent VTE was numerically lower in the apixaban compared with the dalteparin group (5.6 percent vs 7.9 percent; hazard ratio [HR], 0.63, 95 percent confidence interval [CI], 0.37–1.07; p<0.001 for noninferiority, p=0.09 for superiority). [ACC.20, abstract 20-LB-20401-ACC; N Engl J Med 2020;doi:10.1056/NEJMoa1915103]
This reduction was mainly due to the decrease in recurrent PE (3.3 percent vs 5.5 percent; HR, 0.54). The incidence of recurrent DVT was 2.3 and 2.6 percent in apixaban and dalteparin recipients, respectively (HR, 0.87). There were four and three incidents of fatal PE among apixaban and dalteparin recipients, respectively.
Incidence of major bleeding was similar between apixaban and dalteparin recipients (3.8 percent vs 4.0 percent; HR, 0.82, 95 percent CI, 0.40–1.69; p=0.60). This applied to both major gastrointestinal (GI) bleeding (1.9 percent vs 1.7 percent; HR, 1.05) and major non-GI bleeding (1.9 percent vs 2.2 percent; HR, 0.68).
“This is the only trial in cancer-associated thrombosis where a DOAC is not associated with increased GI bleeding, in spite of the inclusion of a substantial proportion of GI cancers,” noted Agnelli.
The incidence of clinically relevant non-major bleeding was numerically higher in the apixaban vs dalteparin group (9.0 percent vs 6.0 percent; HR, 1.42), and occurred primarily in the upper airways and genitourinary system in apixaban recipients.
All-cause mortality rate at day 210 was 23.4 and 26.4 percent of the apixaban and dalteparin groups, respectively, and was primarily cancer related (85.2 and 88.2 percent, respectively). In each group, four deaths occurred due to VTE and two due to bleeding. The bleeding-related deaths in the apixaban group occurred >3 days after drug discontinuation. Event-free survival over the study period – defined as the absence of recurrent VTE, major bleeding, or death – was greater in the apixaban compared with the dalteparin arm (73.3 percent vs 68.6 percent).
Clinical implications
“VTE is a major cause of complications and death in patients [with cancer], and the high risk of recurrent blood clots and bleeding in [these] patients makes anticoagulant treatment challenging,” said Agnelli, highlighting the importance of research in this specific population.
“Major guidelines recommend low-molecular-weight heparin and have recently added edoxaban and rivaroxaban [though] the clinical benefit of these oral agents is limited by the high risk of bleeding, mainly occurring at GI sites,” he said.
“Findings of Caravaggio expand the proportion of patients with cancer-associated thrombosis who are eligible for treatment with DOACs, including patients with GI cancer,” he added.
What’s next?
The difference in efficacy between dalteparin and apixaban occurred at approximately 30 days into treatment, the point of dalteparin dose reduction.
“It is uncertain whether this divergence suggests that continuing with the initial dose of dalteparin might have improved the efficacy of this agent, a possible benefit that must be balanced with the potential increase in bleeding,” said Agnelli and co-authors.
Additionally, a subgroup analysis showed that patients aged <65 years incurred a greater improvement in VTE risk reduction with apixaban vs dalteparin, a finding which should be further explored, they said.
The authors noted that the findings do not extend to patients with cancers that were excluded from the trial. Furthermore, the study was not powered to assess the bleeding endpoint.