Glycated haemoglobin (HbA1c) levels appear to be an independent predictor of coronary artery disease (CAD) in patients with ST-elevation myocardial infarction (STEMI), a new study has found.
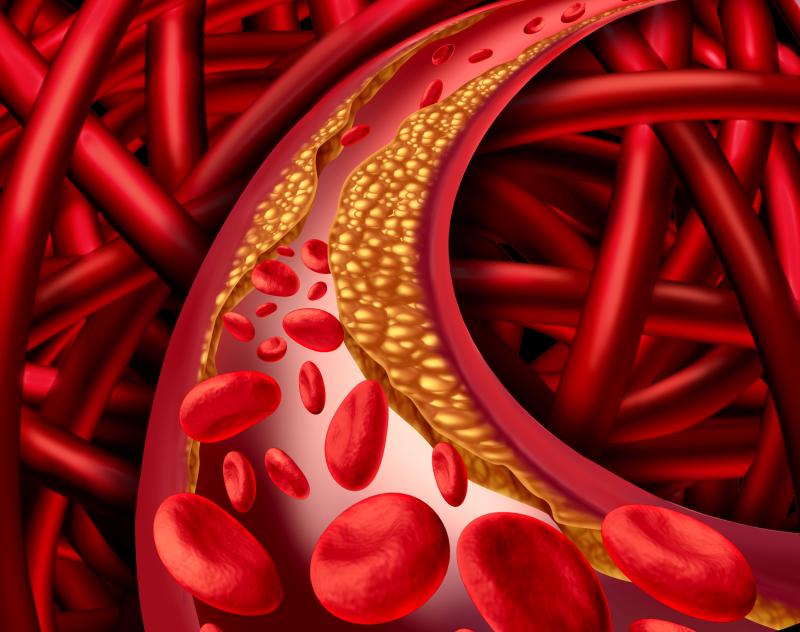
The researchers conducted a cross-sectional analysis of 8,370 STEMI patients with available HbA1c measurements. The study outcome was CAD, as defined by coronary angiogram performed upon admission. Lesions with ≥50-percent-diameter stenosis in the left main coronary artery or in three major coronary arteries was defined as a multivessel disease (MVD).
Of the participants, 4,972 (mean age, 62.32±11.92 years; 82.33 percent male) did not have diabetes mellitus, while the remaining 3,398 (mean age, 60.91±13.13 years; 74.87 percent male) did.
Multivariable analysis found that diabetics were at a significantly higher risk of tachycardia (odds ratio [OR], 1.40, 95 percent confidence interval [CI], 1.21–1.61), of a higher Killip class (OR, 1.12, 95 percent CI, 1.01–1.25) and of MVD (OR, 1.42, 95 percent CI, 1.27–1.58).
HbA1c showed a similar effect, significantly correlating with a greater likelihood of tachycardia (OR, 1.11, 95 percent CI, 1.07–1.15) and MVD (OR, 1.11, 95 percent CI, 1.07–1.15). Risk estimates were calculated for every 1-percent increment in HbA1c.
Using the standard HbA1c cutoffs in clinical practice, researchers continued to find correlations between diabetes and CAD outcomes. HbA1c levels ≤6.5 percent, for example, significantly increased the risk of MVD, as did concentrations exceeding 7 percent.
“[F]or post-MI patients with DM and other comorbidities, physicians may use the number of stenosed vessels to improve cardiovascular risk assessment, and consider more intensive and individually tailored glycaemic control,” said researchers