Hormonal contraceptive + TDF-based ART a recipe for bone disaster in young HIV+ women?




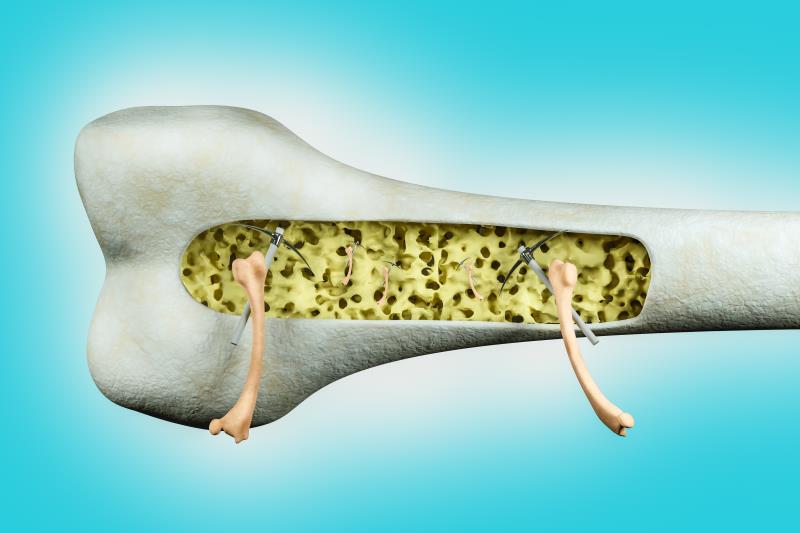
The concomitant use of depot medroxyprogesterone acetate (DMPA) in young women with HIV initiating an antiretroviral therapy (ART) regimen containing tenofovir disoproxil fumarate (TDF) may lead to worsening of bone mineral density (BMD) loss, data presented at AIDS 2020 have shown.
“ART initiation with TDF is associated with BMD loss. Among women of reproductive age, DMPA also negatively impacts BMD … [Our findings show that] concomitant DMPA use was associated with a doubling of BMD loss in young women initiating TDF-containing ART,” said the researchers.
A total of 265 HIV-positive, ART-naïve women (median age 26 years) initiating TDF-based ART were recruited from 11 HIV facilities and general healthcare centres in Kampala, Uganda. Of these, 159 were on DMPA while the rest were not on hormone therapy. A control arm comprising 69 HIV-negative women was also included in the analysis. [AIDS 2020, abstract OAB0105]
The annual rates of BMD loss across all anatomical sites assessed were greater among the HIV-positive women who were on DMPA vs those who were not using hormones (–4.0 percent vs –1.8 percent [lumbar spine], –2.1 percent vs –0.9 percent [total hip], and –2.5 percent vs –1.0 percent [femoral neck]; p<0.05 for all).
A similar trend was observed between HIV-positive women on DMPA and those who were HIV-negative (–4.0 percent vs 0.8 percent [lumbar spine], –2.1 percent vs –0.0 percent [total hip], and –2.5 percent vs 0.1 percent [femoral neck]; p<0.05 for all).
These data reflect the combined deleterious effects of DMPA and TDF initiation on BMD in young women with HIV, the researchers pointed out.
Taking an alternate route with TAF
Evidence has shown an association between TDF use and increased fracture risk, which could either be due to the direct impact of TDF on bone, altered vitamin D metabolism, and/or proximal tubule dysfunction. [Curr Opin HIV AIDS 2016;11:326-332]
There is growing literature attesting to the advantages of ART regimens containing tenofovir alafenamide (TAF) over TDF-based regimens in terms of bone safety without compromising antiviral efficacy. [J Acquir Immune Defic Syndr 2014;67:52-58; Lancet 2015;385:2606-2615; J Acquir Immune Defic Syndr 2015;69:439-445; Lancet Infect Dis 2016;16:43-52]
As such, the findings appear to suggest that it might be worth looking into the potential of TAF-based regimens, as well as alternative contraceptive methods, in this cohort of women to achieve favourable virologic and bone outcomes, underscored the researchers. “Newer … bone-sparing regimens like TAF-based ART may mitigate BMD loss and early ageing among HIV-infected women,” they said.