Adding endothelial shear stress to stenosis severity may improve prediction of abnormal PET result




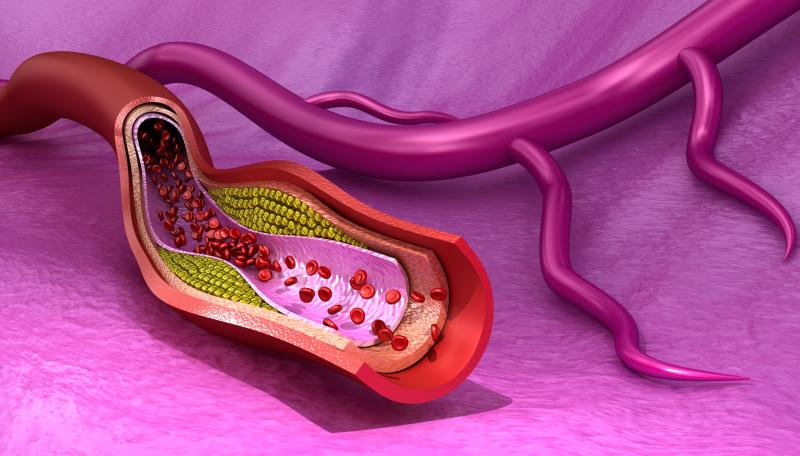
A low-to-moderate positive association exists between lesion plaque burden (PB) and indices of endothelial shear stress (ESS), a recent study has shown. ESS, like PB, increases with stenosis severity and is higher in lesions paired with abnormal positron emission tomography (PET) results.
“ESS is a moderate predictor of impaired vasodilating capability, performing equally with PB and stenosis severity,” the researchers said. “The addition of ESS to stenosis severity can improve prediction of an abnormal PET result.”
C. Anagnostopoulos from the Academy of Athens Biomedical Research Foundation in Greece led the team of researchers which investigated the association of local ESS with PB and with stenosis severity, as well as their comparative performance in predicting impaired coronary vasodilating capability assessed by PET myocardial perfusion imaging (MPI). Results of the study were presented at the ESC Congress 2020: The Digital Experience (ESC 2020).
Forty-nine patients (mean age, 65.3±6.3 years; 29 males) who underwent PET-MPI with 15O-water or 13N-ammonia and computed tomography coronary angiography (CTCA) participated in the study. Abnormal PET was defined as >1 contiguous segment showing both stress Myocardial Blood Flow ≤2.3 mL/g/min and Myocardial Flow Reserve ≤2.5 for 15O-water or <1.79 mL/g/min and ≤2.0 for 13N-ammonia, respectively.
Stenosis severity on CTCA was classified as follows: <30 percent, 31–50 percent, 51–70 percent, and 71–90 percent. The researchers then applied computational fluid dynamics to every vessel, assuming a mean pressure of 100 mm Hg as the inlet boundary condition and a coronary velocity profile of 1 ml/sec as the outlet. They also calculated ESS for the full length of a stenosis (total) and in the proximal (prox), minimum lumen area (MLA), and distal (dist) stenotic segments. Atherosclerotic PB was defined as lesion plaque volume/lesion vessel volume x100.
Evaluation of 85 coronary vessels showed a positive correlation between ESS and PB (r[total]=0.544; r[prox]=0.528; r[MLA]=0.529; r[dist]=0.474; pall<0.001). Stenosis severity resulted in a progressive increase in all ESS indices and PB as compared to segments with a <30-percent stenosis (p≤0.004 for all comparisons). PB and ESS indices were also higher in lesions with impaired vasodilating capacity as compared to those without (p≤0.02 for all comparisons). [Anagnostopoulos C, et al, ESC Congress 2020]
Moreover, all ESS indices demonstrated equal performance with PB and stenosis >50 percent in predicting an abnormal PET-MPI (area under the curve [AUC], from 0.682 to 0.780; p-diff>0.05 for all comparisons.
The predictive ability of the model was increased with the pairwise combination of stenosis >50 percent with the ESS segments (except the distal one) over stenosis alone (AUC [stenosis >50 percent+ESS(total)]=0.80; AUC [stenosis >50 percent+ESS(prox)]=0.797; AUC [stenosis >50 percent+ESS(MLA)]=0.822; p-diff ≤0.01 for all comparisons; AUC [stenosis >50 percent+ESS(dist)]=0.768; p-diff=0.07).
“Advances in CTCA imaging enable assessment of coronary plaque burden, a predictor of myocardial perfusion abnormalities and more recently, with the use of CFD of ESS, an established contributor to atherosclerotic plaque development and progression,” the researchers noted.