
Infertility is a problem faced by 5-10 percent of couples, with male factor accounting for up to 47 percent of cases. [Int J Androl 1987;7(Suppl):1]. There are many causes for male infertility but up to 15 percent of cases are idiopathic in nature. These cases may be related to unregulated excessive oxidative stress, which may impair spermatogenesis; hence, arousing research into the role of antioxidant supplementation in improving the sperm parameters.
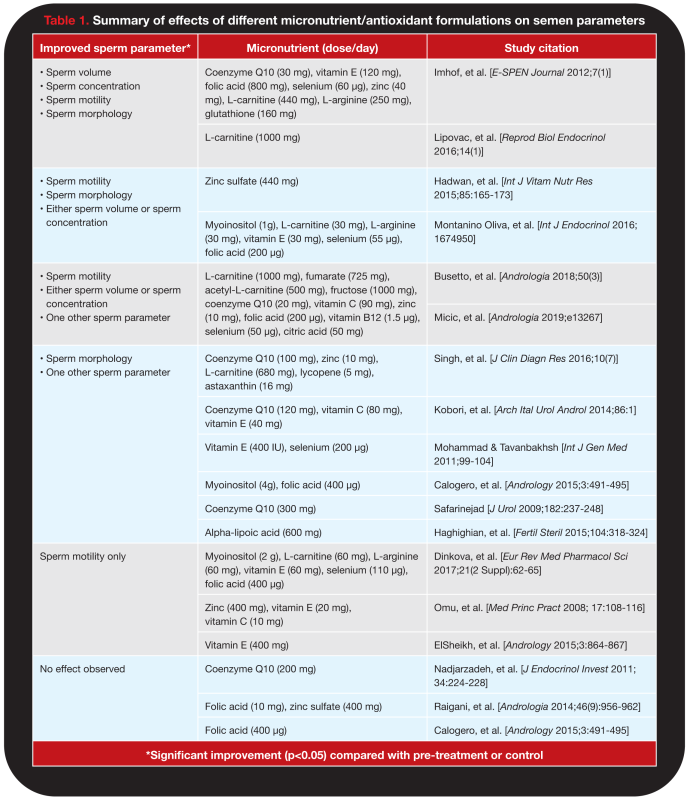
To evaluate the updated literature on the effects of antioxidant supplementation on sperm parameters, Dr Chew Yi Jie (Singapore General Hospital), Dr Janice Tung (KK Women’s and Children’s Hospital), and Associate Professor Tan Thiam Chye (KK Women’s and Children’s Hospital and Duke NUS Medical School) conducted a review of literature published from 2008 to 2019. This review included randomized controlled trials, non-randomized controlled trials and prospective longitudinal studies involving male patients with idiopathic abnormal sperm parameters (volume, concentration, motility, morphology) treated with supplementation of micronutrients and antioxidants for at least 12 weeks. Seventeen studies were included, which are summarized in Table 1.
Alpha-lipoic acid
Only one study evaluated the effect of alpha-lipoic acid (ALA). This was a triple-blind, randomized, placebo-controlled clinical trial that included 44 male patients with untreated idiopathic asthenozoospermia who received either ALA 600 mg daily or placebo. After 12 weeks, those who received ALA had improved sperm count (77.88 million/mL vs 90.43 million/mL; p<0.001), concentration (22.63 million/mL vs 26.35 million/mL; p<0.001), and motility (35.1 percent vs 40.65 percent; p=0.004). [Fertil Steril 2015;104:318-324]
Carnitine
Eight studies evaluated supplements containing carnitines (L-carnitine, acetyl-L-carnitine). All of these studies reported significantly improved sperm motility; six studies reported improvements in sperm concentration; five reported improvements in sperm volume; and five reported improvements in sperm morphology, compared with either controls or baseline levels.
Coenzyme Q10
Seven studies evaluated supplements containing coenzyme Q10. Most of the studies reported improved sperm motility and/or concentration compared with controls or baseline. Fewer studies reported improvements in sperm volume and morphology.
Two studies enrolled patients with idiopathic oligo-astheno-teratozoospermia (OATS). A small study that randomized patients to either coenzyme Q10 200 mg/day (n=23) or placebo (n=24) found no significant differences in the sperm parameters between the two groups. [Endocrinol Invest 2011;34;224-8] However, a larger prospective longitudinal study enrolled 169 patients with idiopathic OATS who received coenzyme Q10 120 mg, vitamin C 80 mg, and vitamin E 40 mg daily for 6 months. Patients experienced significant improvements in sperm concentration (26.3 million/mL vs 49.0 million/mL; p<0.001) and motility (25.2 percent vs 41.3 percent; p<0.001) from baseline to month 6, but not in sperm morphology and semen volume.[Arch Ital Urol Androl 2014;86:1]
Myoinositol-based combinations
Three studies evaluated myoinositol-containing preparations, all of which showed improvements in sperm motility while two studies showed improvements in sperm concentration. In the only randomized, placebo-controlled study, 2 g of myoinositol with 200 μg of folic acid twice daily was associated with significant improvements in sperm concentration (20.2 million/mL vs 26.4 million/mL), total sperm count (46.6 million/mL vs 57.6 million/mL), and progressive motility (22.2 percent vs 27.6 percent). [Andrology 2015;3:491-495] The control group showed no improvement across all studied sperm parameters.
Vitamin E with selenium
Seven studies investigated supplements with either vitamin E, selenium or both, all of which reported improvements in at least one sperm parameter. One longitudinal study found that in 690 male patients with idiopathic astheno-teratozoospermia, daily supplementation of 400 units of vitamin E and 200 μg of selenium for at least 100 days was associated with an increase in motility of at least 5 percent (p<0.05) in 20.5 percent of patients. [Int J Gen Med 2011;99-104]
Zinc
Seven studies evaluated zinc-containing supplements, but only one study investigated zinc monotherapy. In this prospective longitudinal study on 60 patients with idiopathic asthenozoospermia, two capsules of zinc sulfate (220 mg/capsule) daily for 3 months was associated with significant improvements in sperm volume (1.83 million/mL vs 2.39 million/mL; p=0.037), sperm count (47 million/mL vs 70 million/mL; p=0.03), and normal sperm morphology (21 percent vs 33 percent; p=0.041) compared to pre-treatment values. [Int J Vitam Nutr Res 2015;85:165-173]
Conclusion
Overall, the evidence suggests that male patients with idiopathic infertility may benefit from micronutrient/antioxidant supplementation in terms of improving sperm parameters. Sperm motility is most responsive to micronutrient supplementation while sperm morphology is least responsive. Combination therapy confers better outcomes compared with monotherapy.
Investigator’s Perspective
Micronutrient combination therapy associated with better outcomes in semen analysis

Many studies report treatment with antioxidants and micronutrients demonstrated positive improvements in patients with idiopathic abnormal semen analysis results. However, their study designs, study populations, and treatment regimens differ substantially, which makes it challenging to conclude on the effects of specific antioxidants.
Our literature review suggests that amongst the different parameters assessed, sperm motility seems to be the most responsive to micronutrient supplementation while sperm morphology is the least responsive. Furthermore, therapy with a combination of micronutrients is associated with better outcomes in semen analysis compared with monotherapy or dual therapy. However, no study has established the optimal duration of treatment for male patients with idiopathic infertility. There is also a lack of data demonstrating the effect of improvements in sperm parameters on subsequent successful conception, both natural and assisted, as none of the studies reviewed considered live pregnancies as the primary outcome.
Clinicians should be aware that statistically significant improvements in sperm parameters may not translate to clinical significance. These gaps in evidence should be explored in future studies.
Majority of studies used the World Health Organization guidelines for the reference limits of the different sperm parameters, which do not include a considerably large group of men from China, India, Africa, the Middle East, and South America. [Urology 2012;79:16-22] Hence, these reference limits may not be an accurate representation of the worldwide population.
Infertility is a pressing issue that can bring considerable stress to a couple. Male patients, with no known cause of infertility, may benefit from micronutrient/antioxidant supplementation, especially combination preparations, to improve sperm parameters. Treatment responses should be monitored regularly (eg, every 3 months) and interventions adjusted appropriately on an individualized basis.