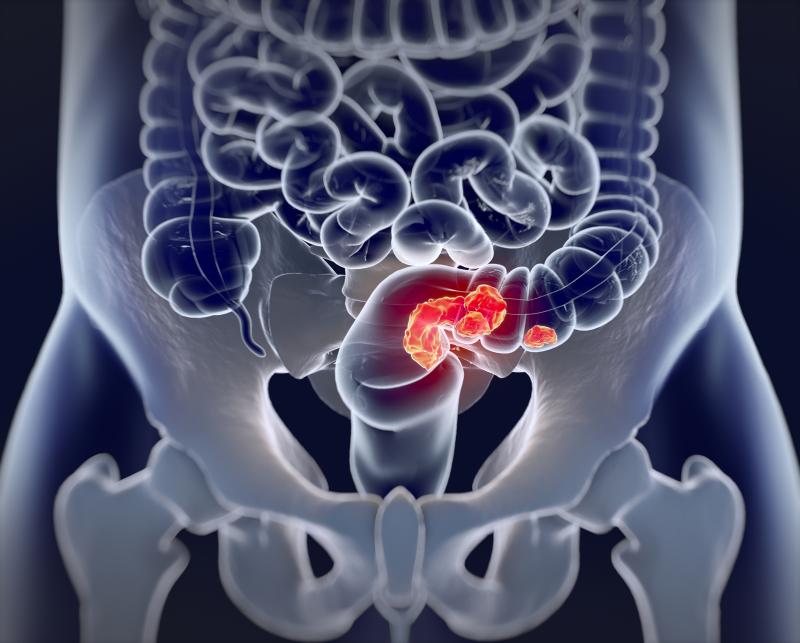
The bevacizumab biosimilar BE1040V for the treatment of metastatic colorectal cancer (mCRC) has met the noninferiority margin in a phase III trial.
“The main purpose of expanding the development of biosimilars is to increase patients' access to biologic therapies… By demonstrating biosimilarity between a reference medicine that has already been approved and a proposed, highly similar medicine, patients would have more access to essential biologic drugs with more affordability,” according to the investigators.
“Furthermore, biosimilars offer benefits to healthcare professionals and healthcare systems as well; by delivering the same outcomes, biosimilars have the potential of imposing significantly less healthcare-related financial burden,” they added. [https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-similar-biological-medicinal-products-containing-monoclonal-antibodies-non-clinical_en.pdf; https://www.igbamedicines.org/]
In the current trial, 126 colorectal cancer patients (mean age, 56.26 years; 63.49 percent female) with evidence of ≥1 metastasis were randomized to receive 5 mg/kg intravenous infusions of BE1040V (n=82) or the reference drug (n=44) plus FOLFIRI-3 every 2 weeks for 1 year. The FOLFIRI-3 regimen comprised irinotecan (100 mg/m2 as a 60-min infusion) and leucovorin (400 mg/m2) on day 1, fluorouracil (2,000 mg/m2 as a 46-h infusion) on day 1 after administration of the previous drugs, and repeat irinotecan infusion on day 3.
BE1040V proved to be as effective as the reference drug in terms of the primary endpoint of progression-free survival (PFS; 7.7 vs 7 months; hazard ratio [HR], 0.79, 90 percent confidence interval [CI], 0.46–1.35; p=0.47). [Clin Ther 2020;doi:10.1016/j.clinthera.2020.03.009]
Likewise, there were no significant between-treatment differences in overall survival (HR, 0.99, 95 percent CI, 0.55–1.80; p=0.99), time to treatment failure (median, 73 days with both drugs; HR, 1.11, 95 percent CI, 0.76–1.61; p=0.59) and objective response rate (difference, 0.19, 95 percent CI, −0.04 to 0.41; p=0.173).
Finally, safety analysis showed no statistically meaningful differences between the biosimilar and reference arms. The rates of grade 3/4 adverse events (AEs) were 23.75 percent and 27.27 percent, respectively. AEs of special interest included haemorrhage (3.75 percent and 2.27 percent), hypertension (13.75 percent and 11.36 percent) and proteinuria (22.5 percent and 27.27 percent), consistent with those reported in previous studies. [J Clin Oncol 2008;26:2013-2019; Chin J Cancer 2011;30:682-689]
“In the immunogenicity assessment, since there were only two reports of a positive result, statistical analysis could not be performed; nonetheless, it seems unlikely that these positive results had a meaningful impact on the study endpoints. This result is in line with the 0.6-percent positive report in clinical trials of adjuvant treatment of a solid tumour with bevacizumab,” the investigators noted. [https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=939b5d1f-9fb2-4499-80ef-0607aa6b114e]
Overall, the present data demonstrate “the noninferior efficacy and comparable tolerability of the biosimilar drug BE1040V compared to the bevacizumab reference drug in mCRC treatment,” they said.
Bevacizumab is indicated for first- or second-line treatment of mCRC in concurrent use with fluorouracil–based doublets. The drug has been approved for use in the second-line setting following progression on a first-line treatment regimen containing bevacizumab. [Semin Cutan Med Surg 2009;28:77-85]