BPA exposure tied to increased asthma symptoms in children




Exposure to bisphenol A (BPA) is associated with increased asthma morbidity among children from predominantly low-income neighbourhoods — particularly in boys, a recent study suggests.
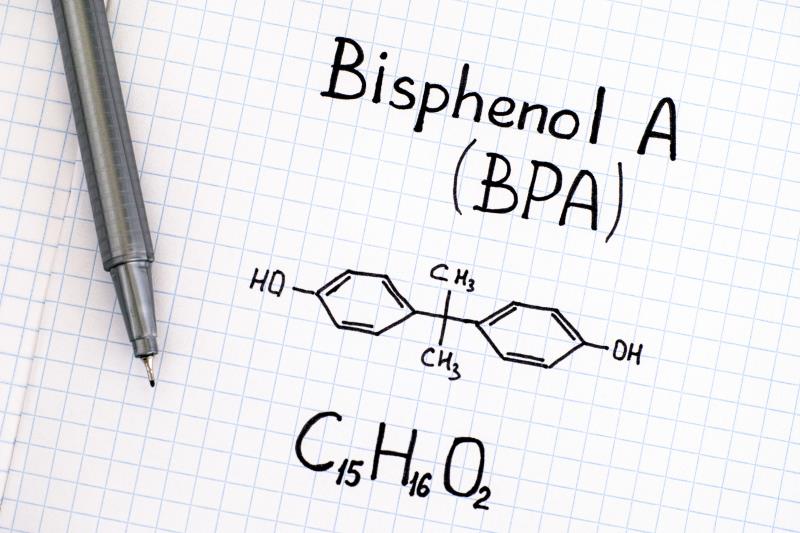
BPA is still widely present in consumer goods, including canned food linings, plastic water bottles, plastic dining wares, toys, and dental sealants, although certain products such as baby bottles no longer contain the chemical.
Widespread exposure due to its pervasive use raises concerns, especially during childhood.
“BPA is a xenoestrogen, and concerns exist that environmental contaminants with endocrine-disrupting properties could play a role in the development or exacerbation of allergic diseases such as asthma,” the researchers pointed out.
In the prospective study of 148 children, BPA exposure was consistently associated with measures of asthma morbidity.
For every 10-fold increase in BPA concentration, the odds of general symptom days raised by 40 percent (adjusted odds ratio [aOR], 1.40, 95 percent confidence interval [CI], 1.02–1.92). [J Allergy Clin Immunol 2020;doi:10.1016/j.jaci.2020.05.031]
Similarly, increases in both maximal symptom days (aOR, 1.36, 95 percent CI, 1.00–1.83) and emergency department visits (aOR, 2.12, 95 percent CI, 1.28–3.51) were also seen for each 10-fold elevation in BPA concentration.
Of note, the strength of associations differed by sex. The associations with BPA concentrations were only significant among boys for symptom days and healthcare utilization.
In addition, the researchers also looked into two structurally similar BPA analogues — bisphenol F (BPF) and bisphenol S (BPS) — which according to them, may be used to replace BPA in consumer products, including those that were labelled as being BPA-free.
“Findings regarding BPS and BPF did not consistently point to associations with asthma symptoms or health care utilization,” the researchers reported.
BPA exposure was approximated via detection of urinary bisphenols using 660 urinary samples collected from 148 African American children aged 5-17 years (mean age 11.2 years, 57 percent males) with established asthma. A majority of them (69 percent) came from low-income families (household annual income below US$35,000).
“BPA exposure is typically higher … among low-income and African American communities than among other socioeconomic or ethnic groups,” noted the researchers.
“It is thought that reduced access to fresh foods, low food security, and consequential consumption of processed foods (eg, eating canned goods, heating and eating foods from plastic containers with BPA) could play a role,” they explained.
Although the underlying mechanisms mediating the associations remained unclear, previous studies have suggested that BPA could trigger oxidative stress and inflammation.
However, there were no associations between BPA or its analogues and lung inflammation as indicated by FENO*.
“Our findings suggest that additional studies are needed to examine this BPA-asthma link, given the high burden of pediatric asthma and widespread exposure to BPA in the United States,” said lead author Dr Lesliam Quirós-Alcalá from the Bloomberg School of Public Health in Baltimore, Maryland, US.
“If these findings are confirmed in future studies, then avoiding or limiting contact with BPA sources may be advisable for families who have children with asthma,” she added.
Quirós-Alcalá cited storing or heating food in BPA-containing plastic wares and consumption of canned foods as examples of BPA sources.