Camrelizumab outwits chemo for oesophageal SCC




The anti-PD-1 inhibitor camrelizumab demonstrated superior efficacy over chemotherapy (CT) and a tolerable safety profile for advanced/metastatic oesophageal squamous cell carcinoma (OSCC) in Chinese patients, the ESCORT* trial suggests.
OSCC accounts for 90 percent of oesophageal cancers in Asia, with more than half of global cases occurring in China. Advanced/metastatic OSCC has a poor prognosis and limited therapeutic options after first-line therapy. [CA Cancer J Clin 2018;68: 394-424; J Epidemiol 2013;23:233-242]
“Given the high prevalence [and limited] treatment options, there is an unmet need [for] novel efficacious drugs for patients in China … The findings suggest that camrelizumab might represent a novel standard second-line treatment option in [this setting],” said the researchers.
A total of 457 patients** were randomized 1:1 to receive IV camrelizumab 200 mg Q2W or CT (docetaxel 75 mg/m² Q3W or irinotecan 180 mg/m² Q2W). [Lancet Oncol 2020;21:832-842]
Overall survival (OS) was longer with camrelizumab vs CT (median, 8.3 vs 6.2 months; hazard ratio [HR], 0.71; p=0.001), as was duration of response among those who achieved an objective response (median, 7.4 vs 3.4 months; HR, 0.34; p=0.017).
This effect was observed across several subsets, including PD-L1 expression subgroups. Camrelizumab favoured patients with higher (≥1, ≥5, and ≥10 percent) vs lower (<1, <5, and <10 percent) PD-L1 expression levels (HRs ranging from 0.51–0.60 vs 0.71–0.82), implying that PD-L1 expression might not be a solid biomarker for predicting outcomes in OSCC. [Lancet Oncol 2019;20:1506-1517] As such, the link between PD-L1 status and clinical outcomes should be explored, noted the researchers.
Despite the similar median progression-free survival (PFS) rates at data cutoff (1.9 months in each arm), the Kaplan-Meier curves separated dramatically thereafter (6 months, 22 percent vs 4 percent for camrelizumab vs CT, respectively), thus boosting the OS outcomes.
“These improvements … were clinically meaningful, and further support the remarkable activity of PD-1 blockade in patients with advanced OSCC,” they said.
Despite the lower incidence of grade ≥3 TRAEs with camrelizumab vs CT (19 percent vs 40 percent), rates were similar for serious TRAEs (16 percent vs 15 percent) and TRAE-induced discontinuation (7 percent vs 5 percent). More deaths from TRAEs occurred in the camrelizumab vs the CT arm (7 vs 3). “TRAEs were generally manageable with treatment interruption or discontinuation as appropriate, indicating that camrelizumab is well tolerated in [this setting],” said the researchers.
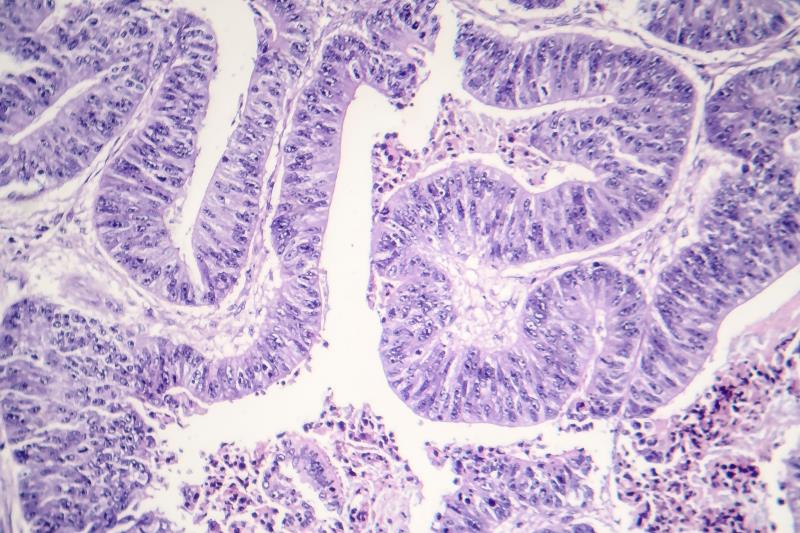
Capillary endothelial proliferation
Of note was the high incidence of reactive cutaneous capillary endothelial proliferation (RCCEP) with camrelizumab (80 percent). “[This immune-related AE is] commonly associated with camrelizumab,” noted the researchers. Nonetheless, regression is likely following withdrawal, which did occur in 62 percent of patients (median time from onset to regression, 6.8 months). Post hoc results showed longer median survival among those with vs without RCCEP (10.1 vs 2.5 months; HR, 0.21).
A higher response rate was seen among camrelizumab recipients who developed RCCEP vs those who did not, suggesting a possible link between RCCEP and tumour response. [Cancer Biol Med 2019;16:173-181] Another study showed a lower incidence of RCCEP with camrelizumab plus the VEGF-receptor 2 inhibitor apatinib vs camrelizumab alone, implicating the role of the VEGFA-VEGFR2 signalling pathway in the pathogenesis of RCCEP.
“We speculate that the balance between enhancers and inhibitors of angiogenesis might be disrupted by the camrelizumab-induced activation of immune response, resulting in the proliferation of capillary endothelial cells,” explained the researchers.
Considering these observations, apart from PD-L1 expression, future trials should explore other biomarkers that might have a hold on outcomes in this setting, said the researchers.