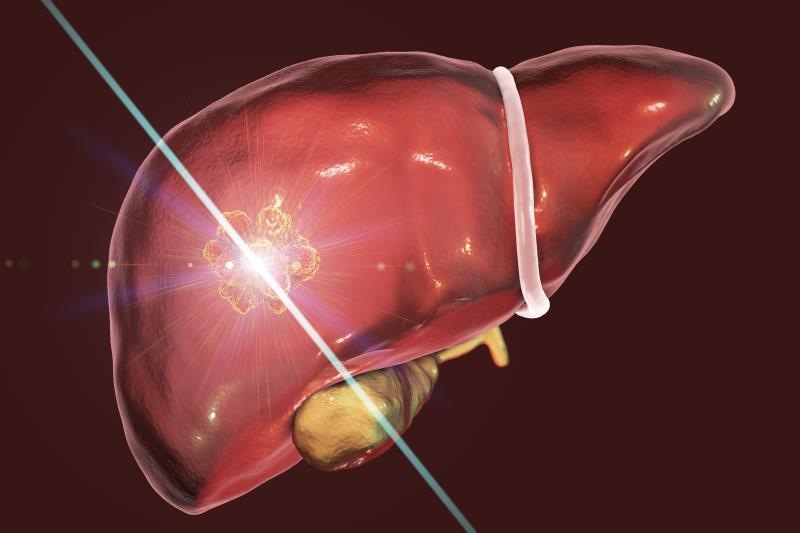
A systematic review and meta-analysis evaluating two percutaneous ablation techniques – microwave ablation (MWA) and radiofrequency ablation (RFA) – showed that the former fared better than the latter in reducing local tumour progression (LTP) rates in individuals with hepatocellular carcinoma (HCC) and/or liver metastases.
Of the 28 studies included (n=3,531), an analysis of 15 observational and three randomized controlled trials (RCTs) showed a significant reduction in the risk of LTP with MWA vs RFA (risk ratio [RR], 0.70, 95 percent confidence interval [CI], 0.53–0.94; p=0.02). This was further reduced when evaluating RCTs only (RR, 0.55; p=0.007). [Onco Targets Ther 2019;12:6407-6438]
A sensitivity analysis excluding studies reporting ‘recurrence’ but not ‘local recurrence’ still favoured MWA over RFA (RR, 0.69, 95 percent CI, 0.51–0.94; p=0.02), further reinforcing the above outcomes.
Impact of tumour size, MWA frequency
Subgroup analyses also showed a reduction in LTP risk among individuals with larger tumours (≥2.5 cm; RR, 0.63; p=0.001), suggesting the influence of tumour size in treatment response. While this finding does not completely discount the benefits of MWA for smaller tumours (<2.5 cm), these results raise the question of whether the LTP reductions with MWA are solely the result of the large tumour effect, the researchers pointed out.
MWA frequency also seemed to factor in, given the significant reduction in LTP risk with a higher vs a lower frequency (2,450 vs 915 MHz; RR, 0.67; p<0.001). “[This] may be explained by the ability of [higher] MWA systems to deliver greater amounts of power and achieve larger ablation volumes … [as] MWA can achieve a penetration of 2.0 cm,” said the researchers. [Future Oncol 2018;14:1755-1764; Ann Surg 2005;242:158-171]
“Larger and more uniform ablation zones with MWA may destroy neoplastic cells more effectively compared with RFA … [Moreover, MWA provides] higher temperatures, faster heating, shorter ablation times … and less heat sink effect [than RFA],” they added.
Feasible alternative to RFA, surgery?
There was no significant difference in the risk of adverse events between MWA and RFA (RR, 1.05; p=0.75 [overall] and RR, 0.84; p=0.68 [four RCTs]). “This finding is important since larger ablations could be perceived to have a higher risk of complications. [Our findings] refute that viewpoint,” said the researchers.
Taken together, these findings are vital in the current HCC treatment landscape, as the current gold standard – surgical resection – is only feasible in the early stages of the disease and among subjects with limited cirrhosis. [Gastroenterology 2016;150:835-853; Ann Oncol 2012;23:vii41-vii48] “[P]ercutaneous ablation has become an important minimally invasive alternative to surgery for liver cancer,” said the researchers.
The findings also support evidence favouring the use of MWA given its reported advantages over the more widely used RFA. [World J Hepatol 2015;7:1054-1063] The improved outcomes associated with MWA and a safety profile relative to RFA reflected in the current study underline the potential of MWA as an alternative to RFA and surgery, noted the researchers.
Further evaluation on the impact of MWA in larger tumours is warranted to ascertain its tissue penetration ability, noted the researchers. Future studies should also look into the treatment cost and time differences between the two ablative modalities, as well as the differences between MWA and nonablative strategies, they added.