In-hospital mortality is comparable but high in both early (EST) and late/very late (LST/VLST) stent thrombosis patients, a recent study has found.
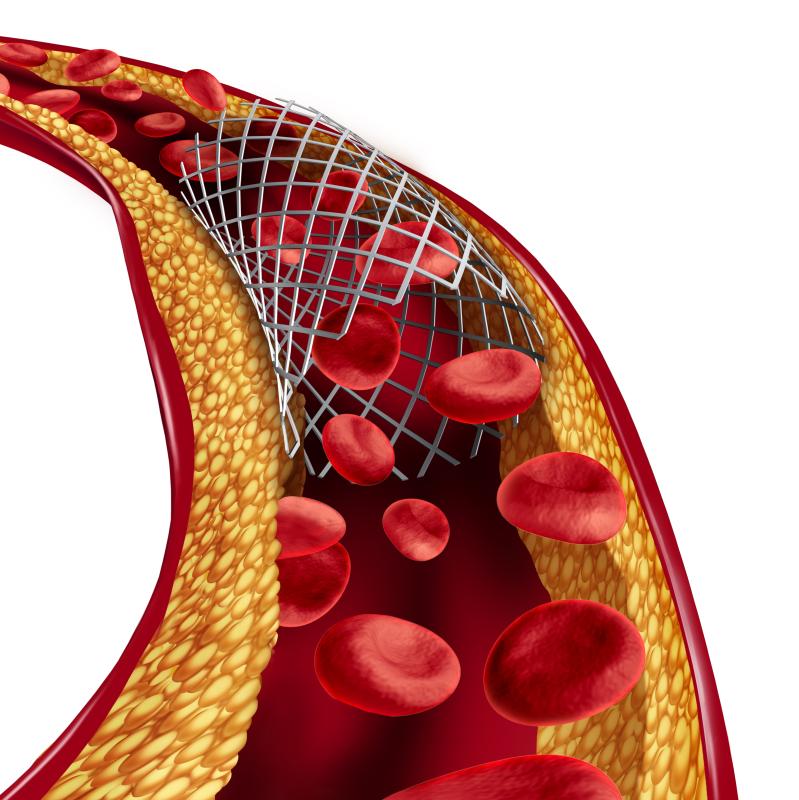
Researchers conducted a comprehensive survey of 370 patients who had received everolimus-eluting stents who developed stent thrombosis. Patients were then categorized according to stent thrombosis timing: ≤30 days (EST: n=287; mean age, 68.5±10.2 years; 80.4 percent male) and 31 to >1 year (LST/VLST; n=83; mean age, 69.2±12.0 years; 81.3 percent male).
Significant differences in patient-related characteristics emerged. Those who were given LST/VLST, for example, more frequently had prior percutaneous coronary intervention (PCI), hypertension, myocardial infarction and haemodialysis. Acute myocardial infarction, peripheral artery disease and current smoking, on the other hand, were significantly more common in the EST patients.
In-stent restenosis also occurred significantly more frequently in the LST/VLST group, while EST participants were more likely to be on dual antiplatelet regimens.
In contrast, treatments and outcomes did not appear to differ between timing groups. Emergency PCI, for example, was performed in 96.1 percent and 100 percent of the EST and LST/VST groups, respectively (p=0.07). Thrombus aspiration was performed in 66.5 percent and 56.1 percent, respectively, and likewise failed to reach statistical significance (p=0.082).
The same was true for balloon dilation (p=0.58), bare metal stent implantation (p=0.88), drug-eluting stent implantation (p=0.44) and emergency coronary artery bypass grafting (p=0.49). The in-hospital mortality rates were 15.0 percent and 21.7 percent in the EST and LST/VLST groups, similarly falling short of significance (p=0.14).