Weight-loss surgery leaves teens deficient in iron, vitamin B12




While bariatric surgery is increasingly recommended in obese teens to achieve significant, sustained weight loss and resolve comorbid diseases, a study has shown a major downside to the procedure: nutritional deficiencies, specifically in iron and vitamin B12.
If left unchecked or inadequately managed, deficiencies in the said nutrients can lead to anaemia, fatigue, exercise intolerance, neurologic dysfunction, and infertility over time. Therefore, lifelong micronutrient supplementation is recommended. [Obes Surg 2017;27:2079-2082; Bone Miner Res 2017;32:1229-1236; Surg Obes Relat Dis 2017;13:727-741]
“Yet, adolescents may be at heightened risk because of low adherence to supplementation and a longer potential lifespan with altered physiology … Our findings underscore the importance of long-term nutritional monitoring in adolescents after bariatric surgery and the need to examine impact on health outcomes and quality of life as these youth advance into adulthood,” the investigators said. [Obesity 2013;21:E190-195]
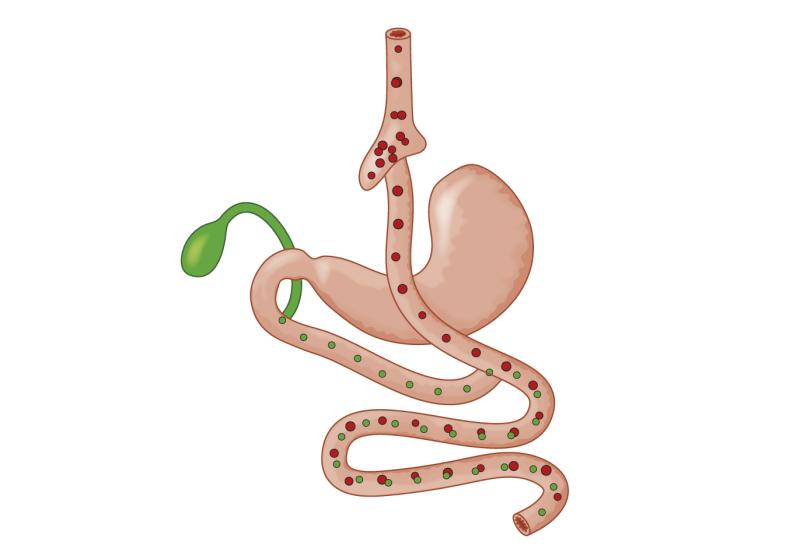
The current 5-year analysis included adolescents (mean age, 16.5 years; 75 percent female who had undergone Roux-en-Y gastric bypass (RYGB; n=161) or vertical sleeve gastrectomy (VSG; n=65) with mean body mass index (BMI) of 52.7 kg/m2 at surgery. Serum levels of ferritin, red blood cell folate, parathyroid hormone (PTH), and vitamins A, D, B1, B12 were measured at baseline and annually.
At year 5, the mean BMI decreased by 23 percent overall, with no significant difference between procedures. Concentrations of vitamin B12 markedly declined, whereas those of transferrin and parathyroid hormone increased in the RYGB but not the VSG group. Ferritin levels dropped significantly in both groups. [Clin Gastroenterol Hepatol 2020;18:1070-1081.e5]
“The most prevalent abnormality we observed was hypoferritinemia, which affected nearly twice as many RYGB recipients by year 5 compared with VSG,” the investigators noted.
The number of patients with hypoferritinemia increased from 2.5 percent at baseline to 71 percent at 5 years in the RYGB group (p<0.0001), and from 11 percent to 45 percent in the VSG group (p=0.002). There were no significant changes in folate or vitamins A, B1, or D levels observed during follow-up.
By year 5, 59 percent of patients in the RYGB group and 27 percent in the VSG group had deficiencies in two or more nutrients. Risk factors for specific deficiencies included surgery type, female sex, black race, supplementation intake, weight regain, and pregnancy for women.
The increased prevalence of iron and B12 deficiencies after RYGB in the present cohort are in line with those reported in a 5-year longitudinal Swedish cohort of obese adolescents. These nutrient deficits are also consistently observed in adults. [Lancet Diabetes Endocrinol 2017;5:174-183; Surg Obes Relat Dis 2017;13:727-741]
“Our study is the first to assess comparative nutritional outcomes in adolescents after both VSG and RYGB. VSG is now the predominant bariatric surgery in adolescents and adults because of limited anatomic alteration, lower operative risk, and presumed lower risk of nutritional deficits,” according to the investigators. “Our results now provide critical evidence that VSG does in fact carry significantly lower nutritional risk than RYGB, but can still worsen iron status.” [Surg Obes Relat Dis 2018;14:1374-1386]
As expected, increased intake of multivitamin supplements led to better nutritional measures, indicating that adequate supplementation and adherence is crucial in this population, they added.
The study was limited by the lack of data on other nutrients including copper, zinc, and vitamin E.