 Mothers are taking the placenta home as it is hailed as a "superfood" for its reduced risk of postpartum depression and increased energy though doctors say the benefits remain unknown.
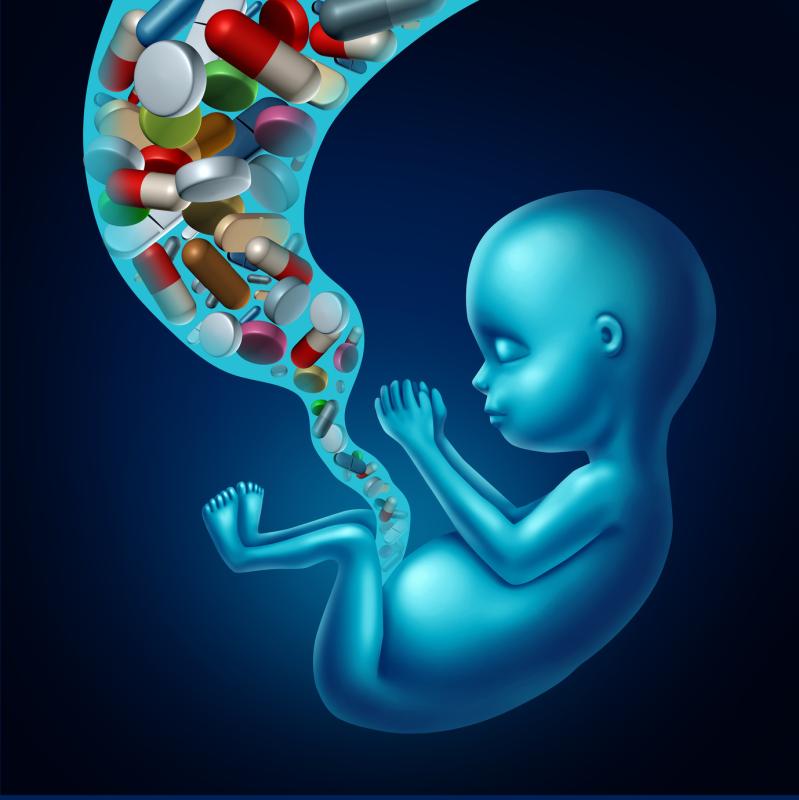
Mothers are taking the placenta home as it is hailed as a "superfood" for its reduced risk of postpartum depression and increased energy though doctors say the benefits remain unknown.Babies born to mothers exposed to high levels of bisphenol A (BPA) during pregnancy are at a greater risk of wheezing and poor lung function, according to a new study presented at the recently concluded International Congress of the European Respiratory Society (ERS 2019).
“Our research doesn’t tell us exactly how the two are linked,” said Alicia Abellan, lead author and postdoctoral researcher at the Barcelona Institute for Global Health, referring to maternal BPA exposure and respiratory health of the baby. “[B]ut previous research in animals has shown that prenatal exposure to BPA can stunt the developing lungs and have an impact on the immune system.”
“It could be that these chemicals interact with hormone signals in the growing baby and alter the correct development of the immune and the respiratory systems,” she added.
Of the 2,685 mothers included in the study, 79 percent had detectable levels of BPA in their urine during pregnancy. Other more uncommon phenols, such as bisphenol S and bisphenol F, were also detected, though in fewer participants. [ERS 2019, abstract OA4969]
In turn, pregnant mothers who had elevated levels of BPA were 13 percent more likely to give birth to babies with wheezing problems than their low-BPA counterparts.
BPA exposure during pregnancy was also implicated in problems with overall respiratory performance in the offspring. When maternal urinary BPA concentrations doubled, it led to a corresponding decrease in infant lung capacity by approximately 5 mL. Lung function was measured in the children participants between the ages of 6 and 10 years.
The researchers included a large sample of mother-children dyads, enrolled from eight different European studies. Despite this, researchers pointed out that an important methodological weakness was that phenol measurements only came from one or two urine samples per pregnant woman, giving investigators only a snapshot of BPA exposure.
They plan to extend the current work by studying how exposure to BPA can affect different patterns of wheezing manifestation across childhood, as well as investigating the potential effects of other phenolic compounds detected in the urine.
“This research suggests that exposure to BPA in the womb may lead to small but measurable differences in children’s lung function,” said Professor Diana Stolz of the University Hospital Basel in Switzerland and Chair of the European Respiratory Society Education Council, who was not involved in the present study.
“These effects might not have much impact on children who are otherwise healthy, but they are very important when we consider the health of a whole population.”
Further studies are needed to more conclusively confirm the relationship between BPA exposure during pregnancy and lung problems in the offspring, she added. The same is true for the potential detrimental respiratory impacts of other chemicals in our environment.