Young gynaecological cancer survivors have an increased risk of bone mineral density (BMD) reductions and osteoporosis, according to a study scheduled for presentation at SGO 20/20.
This retrospective cohort study comprised 185 women aged ≤65 years (median age 55 years, mean body mass index [BMI] 32 kg/m2) who had undergone oophorectomy for uterine or ovarian cancer between the years 2010 and 2014. A majority of the women (78.1 percent) had ovarian cancer. About 78 percent had received chemotherapy and 17.1 percent external beam radiation.
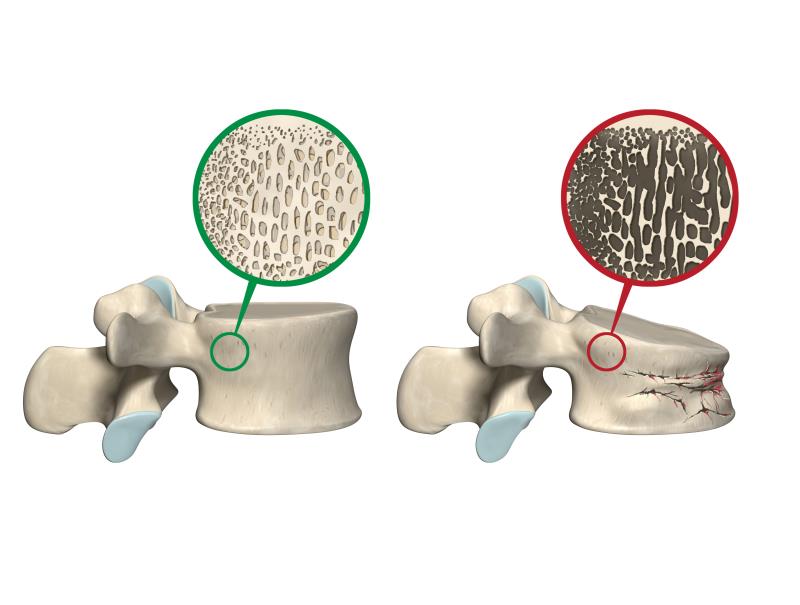
BMD (Hounsfield units [HU]) was assessed based on previous computed tomography (CT) scans at baseline, and at 1, 3, 5, and >5 years following cancer diagnosis. A score of >150 HU was deemed normal, while 100–150 HU suggested osteopenia and <100 HU denoted concern regarding osteoporosis risk.
There was a significant decrease in BMD from baseline throughout the follow-up period (179.4 vs 146.5 HU at 1 year, 176.0 vs 141.9 HU at 3 years, 179.1 vs 140.3 HU at 5 years, and 175.78 vs 123.63 at >5 years; p<0.001 at all follow-up assessments). [SGO 20/20, abstract 130]
Half of the women with normal BMD at baseline had an elevated risk for osteopenia or osteoporosis at 5 years. The risk of osteoporosis also increased over the follow-up period, rising from 4.3 percent at baseline to 7.4 percent at 1 year, 15.7 percent at 3 years, 18.0 percent at 5 years, and 23.3 percent at >5 years.
Several factors were identified as predictors of decreases in BMD. At 1 year, chemotherapy was significantly linked to an increased risk of bone loss (β, 10.9; p=0.03). At 5 years, current smokers had a significantly increased risk of bone loss (β, 52.4; p<0.01). Pre-treatment BMD was a significant predictor of bone loss at all follow-up points (β, 0.7; p<0.01 at 1 year; β, 0.7; p=0.02 at 3 years; β, 0.8; p<0.01 at 5 years).
According to study lead author Dr Janelle Sobecki-Rausch, a fellow in gynaecologic oncology at the University of Wisconsin-Madison, Wisconsin, US, the choice of this study population was to identify survivors of gynaecological cancers who may have an increased risk of osteoporosis earlier in life.
“Adequate treatment of osteoporosis relies on timely and appropriate BMD screening in order to identify those at risk. It is especially important for younger gynaecologic cancer survivors who have a longer life expectancy and may experience premature bone loss from oophorectomy (removal of the ovaries) and chemotherapy,” she said.
“Our data suggest routine BMD assessments within 1 year following initiation of cancer treatment are warranted in this population,” noted Sobecki-Rausch and co-authors.
They also noted that the study demonstrated the feasibility of using CT-based BMD measurements to assess osteoporosis risk in gynaecological cancer survivors.