Minimally invasive pancreatectomy effective for pancreatic neuroendocrine neoplasms




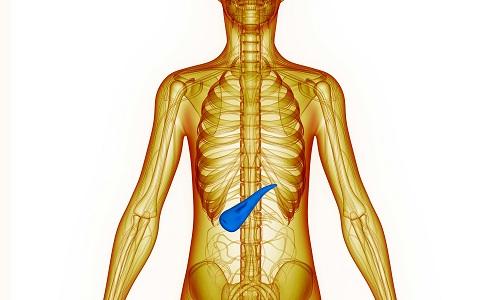
Minimally invasive pancreatectomy (MIP) offers a feasible alternative to open pancreatectomy (OP) for the treatment of pancreatic neuroendocrine neoplasms (PNEN), according to a recent Singapore study has found.
“Postoperatively we found comparable perioperative safety profiles of MIP and OP, with no significant differences in overall morbidity, pancreatic surgery-specific complications, 90-day/in-hospital mortality and readmission rates,” researchers said, however admitting that some intraoperative differences emerged.
The retrospective review included 134 PNEN patients, of whom 36 underwent MIP while 98 received OP. All surgeries were performed with curative intent. Patients and procedures were all enrolled from and performed at the Singapore General Hospital.
After propensity score matching, 35 patients remained in each arm. Those who underwent MIP had significantly longer operating times (mean difference [MD], 75.0 minutes, 95 percent confidence interval [CI], 15.2–134.8; p=0.015), but lower intraoperative bleeding (MD, –400.0 mL, 95 percent CI, –630.5 to –169.5; p=0.001). [Word J Surg 2020;doi:10.1007/s00268-020-05582-3]
Moreover, postoperative outcomes also tended to better in MID patients, who were admitted for a shorter time after the procedure than their OP comparators (MD, –1.0 day, 95 percent CI, –1.9 to –0.1; p=0.029). The median time to diet was also shorter by a day in MID participants (95 percent CI, –1.9 to –0.1; p=0.039).
“These apparent postoperative recovery benefits MIP confers could in part be due to decreased intraoperative bowel handling, improved postoperative pain control and earlier postoperative ambulation,” the researchers said.
The 5-year actuarial overall and disease-free survival rates were calculated to be 83.8 percent and 74.0 percent, respectively. The median time to first recurrence was 19 months, and most recurrences occurred in the liver (63.0 percent). The MIP and OP arms led to comparable likelihoods of overall (hazard ratio [HR], 0.84, 95 percent CI, 0.28–2.51; p=0.761) and disease-free (HR, 0.57, 95 percent CI, 0.20–1.64; p=0.296) survival.
Similarly, no significant between-group differences were reported for short-term adverse outcomes, postoperative complications, in-hospital mortality, readmissions and oncologic clearance.
Some important limitations need to be considered, the researchers said. These include the study’s retrospective nature, small sample size and potential improvements in postoperative care over the two decades that data were collected.
“Nonetheless, to the best of our knowledge, this present study is only the second PSM study comparing MIP and OP for PNEN in the existing literature and the first PSM study to include all PNENs and forms of pancreatic resections,” the researchers noted.
“Future PSM studies with a larger cohort size could examine comparative outcomes between MIP and OP when stratified by the type of pancreatic resection performed,” they added.