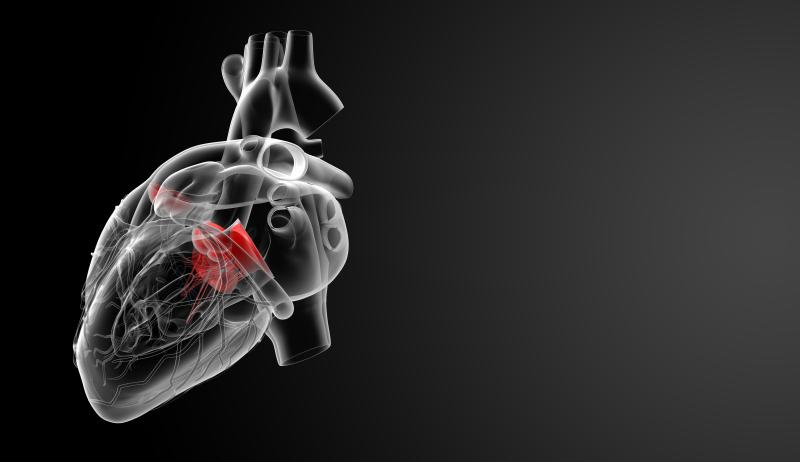
Mitral regurgitation (MR) is more likely to be a comorbidity in patients with the paradoxical low-flow (PLF) severe aortic stenosis (AS) than in those with normal-flow (NF) disease, according to a recent Singapore study.
“Concomitant MR was more common in PLF AS compared to NF AS and may be an important determinant of the low-flow pattern,” said researchers. “Patients with severe AS and concomitant MR demonstrated increased echocardiographic evidence of diastolic dysfunction compared to patients without MR, a trend which was more pronounced in PLF AS compared to NF AS.”
Retrospective analysis of the clinical and echocardiographic profiles of 886 consecutive AS patients showed that most (65.7 percent; n=424) had NF AS; only 221 (34.3 percent) had PLF AS. Moderate or severe MR was more common in the latter group (14.9 percent vs 8.0 percent). [Int J Cardiovasc Imaging 2019;doi:10.1007/s10554-019-01735-1]
Participants across the four groups (PLF AS with or without MR and NF AS with or without MR) were statistically comparable in terms of baseline sociodemographic factors, such as age, sex, blood pressure and heart rate. Body mass index, however, was significantly lower in PLF AS patients with vs without MR (22.8±4.8 vs 25.6±5.4 kg/m2). No such effect was reported for either NF AS group.
The presence of PLF AS correlated significantly with a higher prevalence of concomitant moderate or severe MR relative to NF AS (odds ratio, 2.01, 95 percent confidence interval, 1.21–3.35; p=0.006).
“Our findings were consistent with the hypothesis that for patients with severe AS and preserved left ventricular ejection fraction, the presence of significant MR would be a major determinant of paradoxical low-flow, as the regurgitant flow back to the left atrium in systole would result in reduced flow across the aortic valve,” the researchers said.
Aside from MR, several other important differences between PLF and NF AS were also reported. For instance, left atrial diameter was significantly larger in those with MR, in both the PLF and NF AS groups. No such trend was reported for the left ventricular dimensions, including outflow tract diameter, internal diameter in diastole, relative wall thickness and mass index, among others.
The same was true for diastolic dysfunction. Despite comparable AS severity, diastolic function was poorer in patients with concomitant MR in both patient subgroups. This tended to occur with greater frequency in PLF AS patients.
“Diastolic dysfunction may be difficult to evaluate in the presence of moderate or severe MR as the echocardiographic markers of diastolic dysfunction are often dependent on the mitral inflow,” the researchers said. “For patients with PLF AS and concomitant moderate or severe MR, we had found greater echocardiographic evidence of diastolic dysfunction compared to their NF counterparts.”
“Diastolic dysfunction may precede the development of symptoms and predict progression of disease, and may thus have an important role [in] prognostication and management of patients with underlying severe AS,” they added.
Future studies should focus on identifying the reasons behind the differences between PLF and NF AS, as well as on the potential impacts on treatment.