
Nearly one in four people in Thailand has hypertension (HT), according to the 5th National Health Examination Survey.
From 1992 to 2014, HT prevalence in individuals aged 15 years and older rose from 17 percent to 24.7 percent, with the breakdown showing an increase from 18.1 percent to 25.6 percent in men and from 15.9 percent to 23.9 percent in women. The prevalence also increased with age.
Interestingly, the survey found that the average systolic blood pressure (SBP) in the rural population had a greater increase (114.9 mm Hg to 122.6 mm Hg) than that of the urban population (117.2 mm Hg to 120.8 mm Hg). [The 5th National Health Examination Survey, 2557 (2014). Nonthaburi: Health System Research Institute. Available at: https://kb.hsri.or.th/dspace/handle/11228/1]
The key challenges of treating HT include patients’ lack of awareness regarding their condition and their inability to achieve adequate blood pressure (BP) control within recommended targets. It is estimated that 45 percent of the hypertensive population (approximately 5.8 million people) have not been diagnosed and are unaware of their condition and 6 percent of the hypertensive population (approximately 0.8 million people) have been diagnosed but are untreated. The remaining hypertensive patients are diagnosed and received treatment but only 29.7 percent (approximately 3.8 million patients) managed to achieve a target BP of less than 140/90 mm Hg while 19.3 percent (approximately 2.5 million patients) failed to achieve adequate BP control.
Given these gaps in hypertensive diagnosis and management, the Thai Hypertension Society strongly recommends home blood pressure monitoring (HBPM) for diagnosing and monitoring HT treatment (Level I Recommendation, Quality of Evidence A). Supporting evidence indicates that HBPM contributes to screening for white-coat and masked HT. Moreover, HBPM helps to promote adherence to antihypertensive medications, which leads to better BP control. [2019 Thai Guidelines on the Treatment of Hypertension. Available at http://www.thaiheart.org/images/column_1563846428/Thai%20HT%20Guideline%202019.pdf]
For accurate HBPM measurement, an automated upper arm HBPM device that is accredited by a standards institution should be used. Wrists and finger measurement devices should be avoided unless measuring BP in the upper arm is difficult, for example, in patients with extreme obesity.
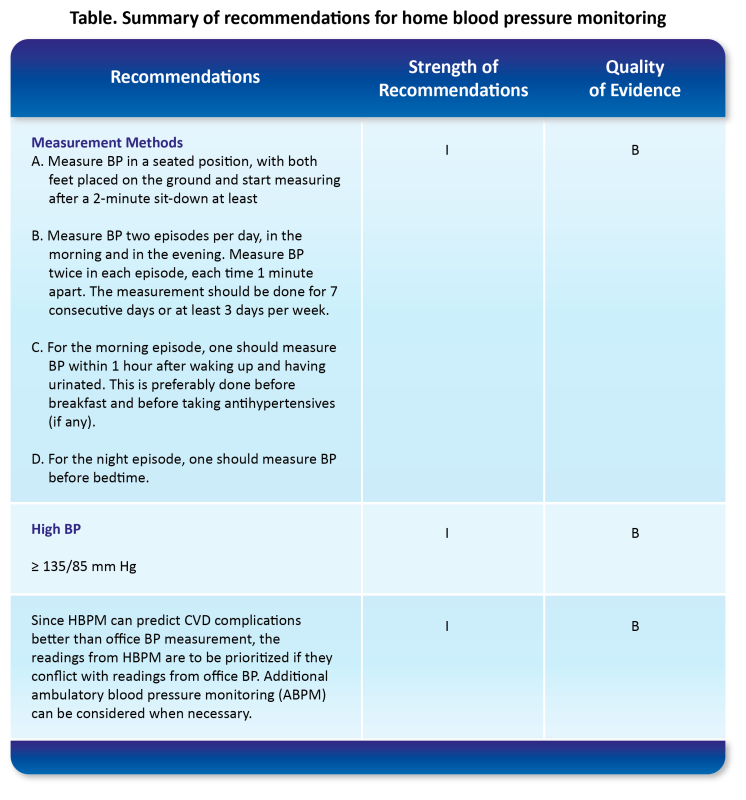
The guidelines have specified the key recommendations for HBPM, including detailed measurement methods and frequency, definition of high BP at home, and the recommendation that HBPM readings should be prioritized if they conflict with the office BP readings [Table]. [2019 Thai Guidelines on the Treatment of Hypertension. Available at http://www.thaiheart.org/images/column_1563846428/Thai%20HT%20Guideline%202019.pdf]
Physicians or healthcare professionals should educate patients and caregivers on the proper use of home BP measurement devices before they begin HBPM. Patients and caregivers should also be advised to keep a record of the BP readings and to bring the records along to the physician for future follow-up.
Consistent HBPM is recommended especially after initiation of antihypertensive medication or following changes in treatment. However, patients should be cautioned against adjusting their medication dose by themselves. As home BP measurement has been observed to be approximately 5 mm Hg lower than office BP measurement, it is recommended to set the target home BP to under 135/85 mm Hg (Strength of Recommendation I, Quality of Evidence B).
Conclusion
Underdiagnosis and undertreatment are major challenges in the treatment of HT in Thailand. The Thai Hypertension Society strongly recommends that HBPM should play a role in the diagnosis and monitoring of HT treatment, and enumerates corresponding methods and targets in the 2019 Thai Guidelines on the Treatment of Hypertension. HBPM may screen for masked or white-coat HT, as well as improve adherence to antihypertensive medication. When used correctly, HBPM readings have been shown to be better predictors of cardiovascular complications than office BP readings and are to be prioritised if conflicts between the two arise.