Comorbidities tied to medication adherence in hypertensive Asians adults




Poor adherence to at least one antihypertensive medication (AHM) is prevalent in an Asian population with hypertension, with comorbidity significantly contributing to medication adherence (MA), according to a Singapore study.
“Concurrent vascular diseases are twice more likely to be associated with poor adherence,” the researchers said. “The comorbidity burden, medication regimen complexity, and AHM drug class did not seem to influence MA.”
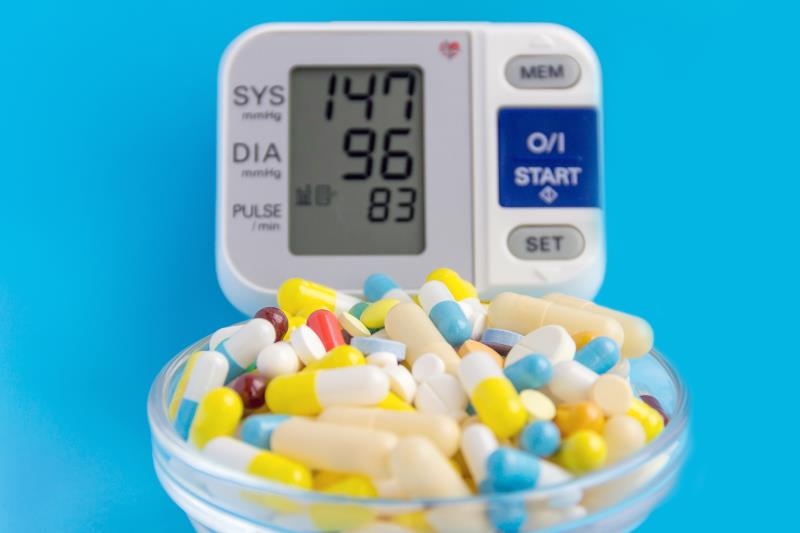
Some 395 Asian adults aged 31–80 years with essential hypertension based on their electronic health records (HER) at a public primary-care clinic completed an assistant-administered questionnaire survey. Data on demographic characteristics, clinical measurements of blood pressure (BP) and body mass index, comorbidities and prescriptions from the HER, and Medication Adherence Report Scale-5 (MARS-5) scores were collated, audited, and analysed.
Poor adherence was defined as a MARS-5 score of <25. Logistic regression analysis was conducted to identify factors associated with adherence to AHM.
Of the patients, 179 (45.3 percent) had poor adherence to at least one AHM. In bivariate analysis, poor adherence significantly correlated with a lower mean age (59 vs 63 years), higher mean clinic diastolic BP (76 vs 73 mm Hg), and higher mean weight (70.4 vs 67.4 kg). [Proc Singapore Healthc 2020;29:167-175]
“At 45.3 percent, the prevalence of poor MA to AHM is significant in this study,” according to the researchers. “This indicates that almost one in two patients are not fully adherent to their AHM.”
Such trend could contribute to the major causes of death in Singapore, which are related to stroke and ischaemic heart disease. This prevalence of poor MA was also consistent with that in other Asian studies, which ranged between 41 percent and 56.5 percent. [www.healthdata.org/Singapore; Patient Educ Couns 2016;99:1894-1900; J Eval Clin Pract 2015;21:166-172; Eur J Cardiovasc Nurs 2013;12:17-24]
In logistic regression analysis, MA was significantly better among patients without any comorbidities, such as diabetes mellitus, dyslipidaemia, stroke, and ischaemic heart disease (odds ratio, 1.98, 95 percent confidence interval, 1.14–3.45; p=0.02). No significant difference in MA was found between the classes, dose frequency, and number of AHM.
“This result contradicts the findings by Calderón-Larrañaga and colleagues, who reported that participants with vascular comorbidity (ie, diabetes, dyslipidaemia, and obesity) were less likely to have poor adherence,” the researchers said. [Int J Cardiol 2016;207:310-316]
Although some studies found better adherence among patients with higher comorbidity scores, several others showed that having more comorbidities was associated with poor adherence. [Am J Manag Care 2010;16:568-576; Eur J Prev Cardiol 2013;20:930-937; J Am Geriatr Soc 2013;60:1298-1303; J Gen Intern Med 2012;27:57-64; Am J Manag Care 2009;15:833-840; Curr Hypertens Rev 2014;10:41-48]
“Physicians should pay attention to patients with comorbidity to assess their adherence to AHM,” the researchers said. “Interventions leveraging on innovations to automate the assessment of MA and alerting the physicians of patients at risk of poor adherence are being developed for future research.”