Among patients with venous thromboembolism (VTE) and active cancer, direct-acting oral anticoagulants (DOACs) are better at preventing VTE recurrence with a lower risk of bleeding compared with warfarin, as shown in a study.
The analysis included a propensity-score matched cohort of a total of 4,976 DOAC users and 4,976 warfarin users with VTE and active cancer. The mean age of the entire cohort was 64 years, and about 49.2 percent of the patients were male. There were 18 percent of patients with history of bleeding, 16 percent with chronic kidney disease, and 5.5 percent who used an antiplatelet.
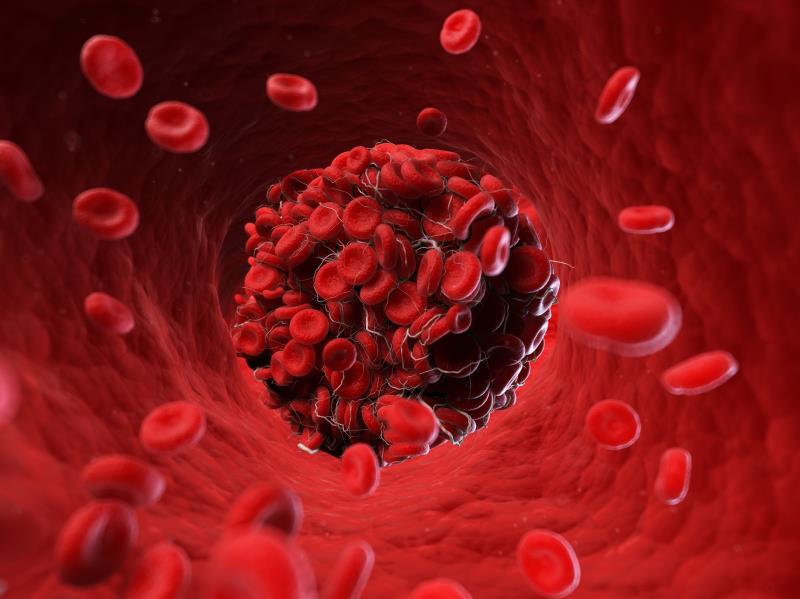
Relative to the warfarin group, the DOAC group had a lower incidence of recurrent VTE (3 vs 5 per 100 person-years) and major bleeding events (2 vs 3 per 100 person-years). Cox regression models confirmed that the use of DOACs was associated with a significantly reduced risk of recurrent VTE (hazard ratio [HR], 0.59, 95 percent confidence interval [CI], 0.42–0.82) and major bleeding events (HR, 0.64, 95 percent CI, 0.44–0.94).
The associations were consistent in an analysis of the comparative effectiveness and safety of the individual DOACs, such that apixaban and rivaroxaban both showed superiority, although the effect of apixaban on the risk of bleeding was not significantly different compared with warfarin.
The present data have important implications, given that thrombotic events are the second leading cause of mortality in patients with cancer, according to researchers.
Overall, the study supports that DOACs—which has a rapid onset of action, short half-life, and convenient route of administration—can be an attractive alternative to warfarin for the secondary prevention of VTE in patients with active cancer who are unwilling or unable to use low-molecular weight heparin, in those aged >65 years, and in cancer types that are considered at high or very high risk of VTE, they added.