Luspatercept reduces transfusion burden in β-thalassaemia patients




Treatment with luspatercept, a recombinant fusion protein that binds to select transforming growth factor β superfamily ligands, led to a significantly reduced transfusion burden* in patients with transfusion-dependent β-thalassaemia, according to a recent study.
This phase III, double-blind trial involved 336 adults with transfusion-dependent β-thalassaemia (median age 30 years, 58.0 percent female) who required regular transfusions (6–20 units of packed red cells within 24 weeks before randomization). Participants were randomized in a 2:1 ratio to receive either subcutaneous luspatercept 1.00–1.25 mg/kg of body weight (n=224) or placebo (n=112) for 48 weeks. All patients received best supportive care, particularly red-cell transfusion and iron-chelation therapy. [N Engl J Med 2020;382:1219-1231]
A significantly higher percentage of patients treated with luspatercept achieved a ≥33 percent reduction in transfusion burden from baseline to week 13–24 (21.4 percent vs 4.5 percent; odds ratio [OR], 5.79; p<0.001) and week 37–48 (19.6 percent vs 3.6 percent; OR, 6.44; p<0.001) compared with placebo.
Significantly more patients who received luspatercept than placebo also had a ≥50 percent reduction in transfusion burden from baseline (week 13–24, 7.6 percent vs 1.8 percent; OR, 4.55; p=0.03 and week 37–48, 10.3 percent vs 0.9 percent; OR, 11.92; p=0.002).
At any 12-week interval of treatment, more patients in the luspatercept arm vs the placebo arm also reported a transfusion burden reduction of ≥33 percent (70.5 percent vs 29.5 percent; OR, 5.69) and ≥50 percent (40.2 percent vs 6.3 percent; OR, 9.95), with a reduction of ≥2 red-cell units.
“[Moreover,] reductions in the transfusion burden of ≥33 percent and ≥50 percent from baseline were estimated to avoid the need for approximately 7 and 8 red-cell units, respectively, per patient over 6 months,” said the researchers.
At week 48, serum ferritin levels were reduced in the luspatercept arm (mean change from baseline, -248 µg/L), while it increased in the placebo arm (mean change from baseline, 107 µg/L). This result also “suggests favourable early effects on iron balance,” the researchers noted.
However, a higher incidence of adverse events (AEs), such as (19.7 percent vs 8.3 percent), arthralgia (19.3 percent vs 11.9 percent), dizziness (11.2 percent vs 4.6 percent), hypertension (8.1 percent vs 2.8 percent), and hyperuricaemia (7.2 percent vs 0 percent), was observed among patients on luspatercept than those on placebo. “Luspatercept was associated with mainly low-grade AEs[, with only few patients discontinuing the treatment],” said the researchers.
Nevertheless, the overall reduction in transfusion burden was substantially greater with luspatercept than placebo. “The response with luspatercept [treatment] was sustained, and multiple episodes of response were observed,” the researchers said.
“[Furthermore,] a 5-year, open-label, extension phase is underway to provide long-term data on the safety of luspatercept and its effects on the transfusion burden and iron outcomes,” they added.
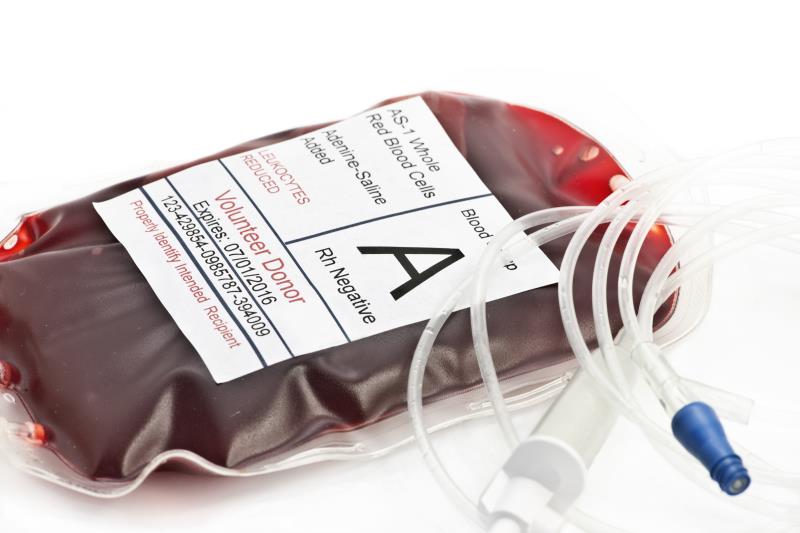
*Transfusion burden: Defined as the total number of red-cell units transfused