A recent retrospective study from Singapore identified several factors associated with a higher risk of mortality following hip fracture, including male sex, older age, and a higher number of comorbidities.
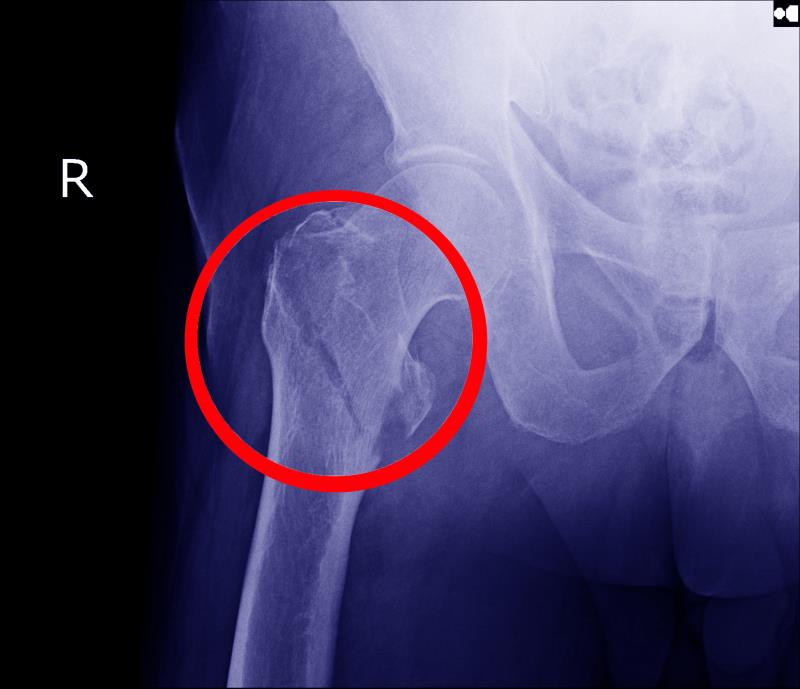
The researchers looked at data of 36,082 individuals aged ≥50 years (mean age 78.2 years, 69 percent female, 84.1 percent Chinese) who had been hospitalized in Singapore for a first hip fracture between 2000 and 2017. A majority of the patients (41.2 percent) had a Charlson Comorbidity Index (CCI) score of 1–3. Trochanteric fractures were the most common type (46.7 percent) followed by cervical fractures (30.7 percent).
Factors associated with a significantly increased risk of mortality after hip fracture were male sex (adjusted hazard ratio [adjHR], 1.46, 95 percent confidence interval [CI], 1.41–1.52), Malay ethnicity (adjHR, 1.23, 95 percent CI, 1.15–1.30 vs Chinese ethnicity), age ≥85 years (adjHR, 5.20, 95 percent CI, 4.27–6.34 vs age 50–54 years), and a higher number of pre-existing comorbidities (adjHR, 3.62, 95 percent CI, 3.42–3.84 for CCI score ≥6 vs 0). [JAMA Network Open 2020;3:e1919706]
Mortality was also elevated among individuals who had trochanteric fractures (adjHR, 1.11, 95 percent CI, 1.06–1.16 compared with cervical fractures), while mortality rate was lower in the more recent years of follow-up (adjHR, 0.59, 95 percent CI, 0.56–0.62 for 2012–2017 vs 2000–2005).
“These findings suggest that interventions to improve outcomes after hip fracture need to focus on patients who are male, are of Malay ethnicity, have higher prefracture comorbidity, and have trochanteric fractures,” noted the researchers.
Absolute mortality after hip fracture reduced over the time periods, by 21 percent in 2006–2011 and by 40 percent in 2012–2017, compared with 2000–2005.
Standardized mortality ratio (SMR) in the first-year after hip fracture reduced among women (SMR, 2.05 [2013–2016] vs 2.54 [2003–2007]) but not men (SMR, 3.28 vs 3.42). Individuals aged 50–64 years had the highest SMR in the first-year post-fracture (SMR, 12.4 and 10.6 in women and men, respectively) compared with individuals aged ≥65 years (SMR, 2.1 and 3.1, respectively).
“Our study provides encouraging results that absolute mortality after hip fracture has decreased over time, as has short-term relative mortality in women,” said the researchers.
“Despite improving absolute mortality outcomes, the elevated mortality risk compared with the general population (SMR) implies that efforts to prevent hip fractures, such as fall prevention and prophylactic medication among elderly individuals with osteoporosis, may be cost-effective by reducing the mortality burden of hip fracture,” they said.
Future research could involve investigating comparative risk of mortality among individuals with and without hip fracture in Singapore matched for CCI score, as well as the reasons for the decrease in SMR in women but not men.