ORF8 and ORF3b antibodies: Highly sensitive and specific new markers for early and late SARS-CoV-2 infection




Hong Kong and French researchers have assessed antibody responses to a panel of 15 severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) antigens, identifying and further validating antibodies to open reading frame (ORF)8 and ORF3b within the virus’s RNA as accurate serological markers of early and late SARS-CoV-2 infection.
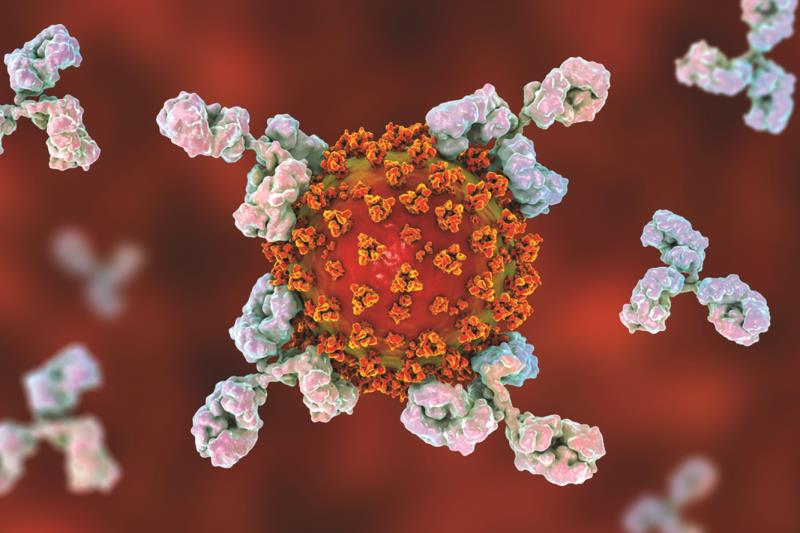
SARS-CoV-2 antibody testing is a major component for diagnosis of recent and past infection. Among the potential antigens, the S structural protein is responsible for viral entry and is widely used as a diagnostic marker of infection. However, patients with coronavirus disease 2019 (COVID-19) produce antibodies to structural and nonstructural proteins beyond the S protein.
The researchers used luciferase immunoprecipitation system (LIPS) to assess antibody responses to a panel of 15 SARS-CoV-2 antigens, representing the structural and nonstructural viral proteins, in 15 patients with COVID-19 and 15 prepandemic negative controls. “The largest difference in mean antibody signals among the [previously uncharacterized] ORFs between COVID-19 samples and negative controls was observed for ORF3b [7,712 ± 2,947 luminometer units (LU) vs 3,599 ± 1,029 LU; p<0.0001] and ORF8 [16,933 ± 7,489 LU vs 5,440 ± 1,096 LU; p<0.0001],” reported the researchers. [Nat Immunol 2020, doi: 10.1038/s41590-020-0773-7]
To evaluate assay performance of ORF3b and ORF8 antigenic targets, they were further validated on a larger panel of sera totalling 84 plasma samples from patients with COVID-19 from early (n=51; <14 days after symptom onset) and late time points (n=33; >14 days after symptom onset) and 176 negative prepandemic controls. “Individually, ORF3b and ORF8 antigens showed high sensitivity levels of 86.6 percent and 100 percent, respectively,” wrote the researchers.
As ORF3b and ORF8 showed the lowest homology to previous SARS-CoV among all the viral proteins, the researchers also looked at the combination of responses towards ORF3b and ORF8. [Microbes Infect 2020;9:221-236] “The ORF3b plus ORF8 sum showed that all patients with COVID-19 had a total score above and all negative controls had a sum below the cut-off, with all early time points being correctly detected … The levels of these antibodies were stable up to day 100 after symptom onset … Therefore, combination use of ORF3b and ORF8 tests could be sufficient to detect individuals exposed to COVID-19 at any time point of infection,” proposed the researchers.
Very little is known about ORF3b and ORF8 function and expression in SARS-CoV-2. Previous reports found that ORF3b of SARS-CoV plays an important role in interaction with the innate immune system through inhibition of type 1 interferon synthesis. [Cell Death Discov 2019;5:101] Recent findings showed that SARS-CoV-2 utilizes ORF8 to alter the expression of major histocompatibility complex I to evade immune surveillance. [preprint at bioRXiv 2020, doi: 10.1101/2020.05.24.111823] “Further investigation into the protective potential of antibodies to these nonstructural targets is needed,” advised the researchers.
“There is a need for improvement of current sero-diagnostic tests for detecting infection early after onset of symptoms, and for confirmatory assays when existing enzyme-linked immunosorbent assay [ELISA] tests for S and N protein-specific antibodies are positive. The combined use of ORF3b and ORF8 provides a highly sensitive and specific method for the detection of COVID-19, both early and late in the course of infection,” concluded the researchers.