Individuals with ulcerative colitis (UC) appear to be at an elevated risk of developing and dying from colorectal cancer (CRC), despite often presenting at an earlier stage of CRC than those without UC, a recent study showed.
The researchers compared CRC incidence and mortality occurring between 1969 and 2017 among 96,447 patients with UC (median age at first diagnosis, 40 years) from Denmark and Sweden with that of 949,207 individuals from the general population of these countries.
CRC incidence was higher among patients with UC than in the comparator group (1.29 vs 0.82 per 1,000 person-years; hazard ratio [HR], 1.66, 95 percent confidence interval [CI], 1.57–1.76), as was CRC-related mortality (0.55 vs 0.38 per 1,000 person-years; HR, 1.59, 95 percent CI, 1.46–1.72). [Lancet 2020;395:123-131]
CRC mortality was comparable between men and women with UC and was highest in individuals diagnosed with UC before age 40, with no increased mortality rates among those diagnosed with UC at age ≥60 years. Similarly, CRC incidence was higher among individuals diagnosed with UC before age 18 years (HR, 37.0), with no increased risk among those diagnosed at age ≥60 years (HR, 0.98).
CRC incidence and mortality were highest in the first year of follow-up, remaining stable after 20 years, and were higher among those with UC for ≥8 years or with primary sclerosing cholangitis compared with those without UC.
According to the researchers, detection or surveillance bias may have partly contributed to the elevated CRC in the first year post-UC diagnosis.
Although patients with UC tended to present at an earlier stage of CRC than those without UC (p<0.0001), CRC-related mortality risk remained greater among patients with UC compared with those without after accounting for tumour stage at diagnosis (HR, 1.54, 95 percent CI, 1.33–1.78).
An analysis of data from the last 5 years of follow-up in Sweden showed a decline in CRC incidence and mortality among patients with UC (incidence: HR, 1.38; mortality: HR, 1.25), which the researchers attributed to improvements in surveillance and treatment and different diagnostic methods or disease classifications.
Room for improvement remains
The higher risk of CRC among those with UC has been noted in the past, leading to the development of surveillance programmes to detect CRC in this group, said the researchers.
However, the present study suggests that the increased CRC incidence and mortality persists despite these programmes and currently available treatments, particularly among those with UC and risk factors for CRC (eg, early-onset UC, extensive colitis, primary sclerosing cholangitis, first-degree relative with CRC).
“Our study shows that screening and treatment of these patients can likely be further improved, since patients with UC are still more likely to die of colon cancer,” said study author Professor Jonas Ludvigsson from Karolinska Institutet, Stockholm, Sweden.
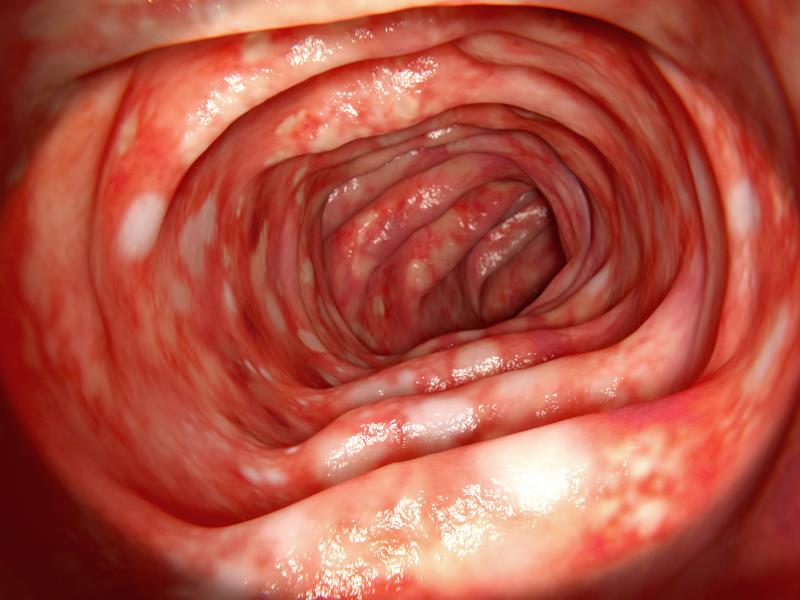
“[T]he findings [also] … highlight the importance of surveillance colonoscopies in any population … to identify dysplasia and prevent the development of CRC altogether. High quality surveillance colonoscopy will ensure appropriate and timely removal of endoscopically resectable lesions before progression to cancer,” said Professor Maria Abreu and Dr Oriana Damas from the University of Miami Miller School of Medicine, Miami, Florida, US, in a commentary. [Lancet 2020;395:92-94]
“We need to develop noninvasive methods for detection of dysplasia, improve training in surveillance techniques for patients with [inflammatory bowel disease], and develop more precise patient-specific surveillance protocols,” they added.
The researchers noted that the study did not account for lifestyle risk factors, some of which may have influenced the findings. Additionally, Abreu and Damas suggested that differences in CRC management between those with and without UC – information of which was unavailable – may have affected survival.