Polymer-free on par with durable polymer drug-eluting stents




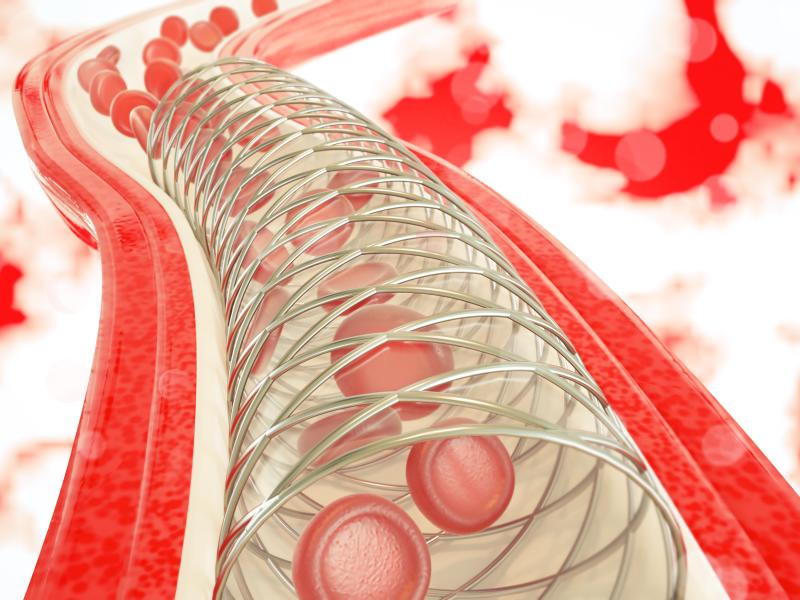
Patients treated with polymer-free drug-eluting coronary stents (DES) show outcomes similar to those treated with durable polymer DES at 10 years, reports a study.
“[T]here were no measurable differences in outcomes between patients treated with a polymer-free sirolimus- and probucol-eluting stent and those treated with a new-generation durable polymer zotarolimus-eluting stent,” the researchers said.
“The incidence of stent thrombosis was low and comparable in both groups, suggesting that differentiating duration of dual antiplatelet therapy after stenting according to the presence or absence of polymer may not be necessary,” they added.
Of the 3,002 patients (median age, 67.8 years) enrolled in this study, 2,002 were randomized to polymer-free sirolimus- and probucol-eluting stents and 1,000 to durable polymer zotarolimus-eluting stents. The composite of cardiac death, target vessel-related myocardial infarction, or target lesion revascularization (a device-oriented composite endpoint [DOCE]) was the primary endpoint.
Secondary endpoints included patient-oriented composite endpoint (POCE), such as all-cause death, any myocardial infarction, or any revascularization; individual components of the composite endpoints; and definite or probable stent thrombosis.
Only 63.9 percent of patients were alive at 10 years. Both groups registered high rates of DOCE and POCE, demonstrating no difference in the incidence between polymer-free sirolimus- and probucol-eluting stents and durable polymer zotarolimus-eluting stents (DOCE: 43.8 percent vs 43.0 percent, respectively; hazard ratio [HR], 1.01, 95 percent confidence interval [CI], 0.89–1.14; p=0.90; POCE: 66.2 percent vs 67.7 percent, respectively; HR, 0.94, 95 percent CI, 0.86–1.04; p=0.22). [J Am Coll Cardiol 2020;76:146-158]
Individual components of the composite endpoints had similar rates in both groups, while the incidence of definite/probable stent thrombosis over 10 years was low and comparable (1.6 percent vs 1.9 percent; HR, 0.85, 95 percent CI, 0.46–1.54; p=0.58).
“Overall cumulative adverse cardiac event rates were high during 10-year follow-up, highlighting an unmet need for further development of secondary prevention measures in patients undergoing coronary stenting,” according to the researchers.
Compared with other clinical trials, which also used zotarolimus-eluting stent as comparator, target vessel revascularization rates observed in the current study were high in both groups. This could be explained by the increased baseline risk of the enrolled patients and the study methodology used. [Circulation 136:1304-1314]
Of note, early-generation DES posed a higher risk of very late stent thrombosis than bare-metal stents, which appeared to be associated with systematically impaired arterial healing after stent implantation. [Arterioscler Thromb Vasc Biol 2007;27:1500-1510]
“The underlying pathogenic mechanisms appeared to be polymer-related inflammatory reaction and endothelial cell dysfunction, which may predispose to more thrombus formation on uncovered struts and, later on, to accelerated de novo atherosclerosis developing within the stented segment, a condition referred to as neoatherosclerosis,” the researchers said. [Eur Heart J 2015;36:2147-2159; J Am Coll Cardiol 2011;57:1314-1322]
“Because of these concerns, polymer-free stent technology has been investigated since early in the development of DES technology. Initial investigations suggested inferior clinical efficacy of polymer-free DES compared with durable polymer DES,” they added. [Eur Heart J 2008;29:1975-1982; Circulation 2004;109:487-493]