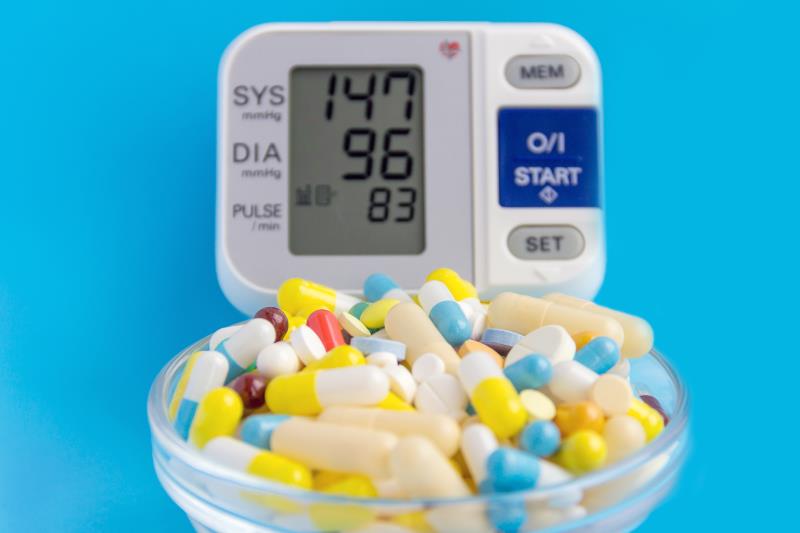
The effect of various antihypertension medications on reducing cardiovascular (CV) risk may differ across drug classes, according to a meta-analysis.
“[A]ngiotensin-converting enzyme (ACE) inhibitors appeared to be the medications of choice to prevent myocardial infarction (MI) and diuretics appeared to be the optimal choice to reduce revascularization,” noted the researchers.
The researchers analysed 46 randomized clinical trials published between 1990 and 2017 assessing antihypertension medications (ACE inhibitors, angiotensin receptor blockers [ARBs], dihydropyridine calcium channel blockers [CCBs], non-dihydropyridine CCBs, β-blockers, and diuretics) with CV event* follow-up for ≥6 months. The resulting population comprised 248,887 non-pregnant adults with hypertension and no major comorbidities** (mean age 65.6 years, 52.8 percent male, mean baseline systolic blood pressure [BP] 161.3 mm Hg). The overall change in systolic and diastolic BP across the trials was a mean -18.0 and -10.1 mm Hg, respectively, and there was a 11.5 percent risk of CV events. A total of 28,658 first-in-trial CV events were reported over a mean 3.7-year follow-up period.
Antihypertension medications were associated with a 17–29 percent reduction in risk of CV events (ACE inhibitors: risk ratio [RR], 0.71; dihydropyridine CCBs: RR, 0.73; β-blockers: RR, 0.83; ARBs: RR, 0.79; and diuretics: RR, 0.73). [JAMA Network Open 2020;3:e1921618]
The reduction in CV death ranged from 15 to 22 percent, with a 20 percent risk reduction with ACE inhibitors or dihydropyridine CCBs (RR, 0.80), 15 percent with ARBs (RR, 0.85), and 22 percent with diuretics (RR, 0.78) compared with placebo.
MI rate was reduced by 20 percent with β-blockers (RR, 0.80), by 21 percent with dihydropyridine CCBs (RR, 0.79), and by 28 percent with ACE inhibitors (RR, 0.72) compared with placebo. Reduction in stroke risk ranged from 19 to 39 percent across the classes (ACE inhibitors: RR, 0.66; dihydropyridine CCBs: RR, 0.61; β-blockers: RR, 0.80; ARBs: RR, 0.69; and diuretics: RR, 0.63, vs placebo). Diuretics reduced the risk of revascularization by 33 percent (RR, 0.67 vs placebo).
Metaregression analysis showed that every 10 mm Hg decrease in systolic BP was tied to a 14 percent reduced risk of CV events, a 13 percent reduced risk of CV death, and a 17 percent reduced risk of stroke, while every 5 mm Hg decrease in diastolic BP was tied to a 16, 14, and 20 percent reduced risk of CV events, CV death, and stroke, respectively.
“ACE inhibitors, dihydropyridine CCBs, and diuretics were associated with similarly significant reductions in the risk of overall CV events and CV death,” said the researchers, though the difference between the effects of various antihypertensive classes in reducing CV events was small.
“[O]ur study can guide first-line medication choices [in line with ACC/AHA*** guidelines],” they added.
The small number of studies in the meta-analysis precluded identification of the impact of other factors (eg, demographic factors) on the association between antihypertension medications and CV events, a subject for future research, noted the researchers. Future studies should also look into the CV effects of combined antihypertension medications, they said.