Ursodeoxycholic acid may prevent post-gastrectomy gallstones in gastric cancer




A daily dose of ursodeoxycholic acid (UDCA) may prevent gallstone formation in patients with gastric cancer who have undergone gastrectomy, suggested results of the PEGASUS-D trial.
The multicentre trial enrolled 521 adults with gastric cancer from Korea who, within 2 weeks of undergoing total, distal, or proximal gastrectomy, were randomized 1:1:1 to receive UDCA (300 or 600 mg/day) or placebo for 52 weeks. Of these, 465 patients were included in the analysis (median age 56 years, 311 men).
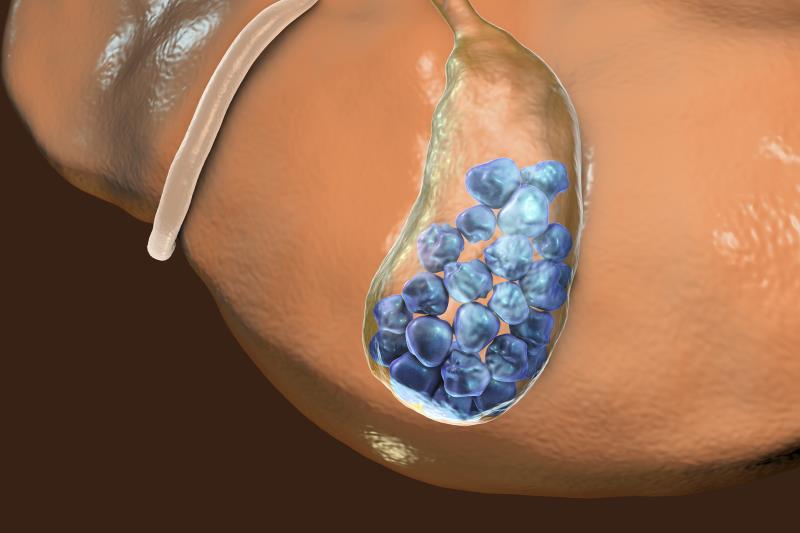
Gallstone formation was assessed every 3 months using ultrasound sonography. Patients with stage ≥2 gastric cancer received adjuvant chemotherapy. Pre-existing gallstones, prior cholecystectomy, biliary infection or obstruction, liver dysfunction, and BMI ≥37 kg/m2 were among exclusion criteria.
Within 12 months of undergoing gastrectomy, fewer UDCA 300 and 600 mg recipients developed gallstones compared with placebo recipients (5.3 percent and 4.3 percent vs 16.7 percent; odds ratio [OR], 0.27, 95 percent confidence interval [CI], 0.12–0.62; p=0.002 [300 mg] and OR, 0.20, 95 percent CI, 0.08–0.50; p<0.001 [600 mg]). [JAMA Surg 2020;doi:10.1001/jamasurg.2020.1501]
Subgroup analysis of patients who underwent D2 lymph node dissection showed a reduction in gallstone formation with UDCA 300 or 600 mg compared with placebo (7.1 percent and 4.1 percent vs 15.1 percent; OR, 0.39; p=0.07 [300 mg] and OR, 0.23; p=0.01 [600 mg]).
Adverse drug reaction (ADR) incidence did not significantly differ between groups (4.7, 1.7, and 1.8 percent of UDCA 300 mg, UDCA 600 mg, and placebo groups, respectively; p=0.18). The most frequent ADRs were nausea (0.8 percent) and skin rash (0.6 percent). There were no serious ADRs. The two deaths that occurred during the study (one each in the UDCA 600 mg and placebo group) were due to cancer recurrence. All gallstone complications that occurred during the study were among placebo recipients (n=4; one case of acute cholangitis and three cases of cholecystitis).
According to the researchers, gallstone occurrence is reportedly more frequent among patients who have undergone gastrectomy compared with the overall population. “[C]holecystectomy is [also] more challenging after gastrectomy because of an increased risk of conversion, bile duct injuries, and longer operating times,” they said. As such, preventing post-gastrectomy gallstone formation is pertinent to prevent additional surgery.
Previous studies have noted the efficacy of UDCA in reducing gallstone formation following bariatric surgery. [J Surg Res 2002;102:50-56; Ann Surg 2003;238:697-702]
“[O]ur study … differs from previous studies in that rapid weight loss is not the main mechanism of gallstone formation,” said the researchers. “[W]e suggest that gallstone formation and its complications may be prevented by the use of UDCA rather than prophylactic cholecystectomy.”
Longer follow-up is warranted to assess the reduction in cholecystectomies and gallstone formation >1 year after gastrectomy, including after UDCA cessation. Generalizability to other ethnicities also remains to be seen.
In a commentary, Professors Henry Pitt and Attila Nakeeb from Temple University, Philadelphia, Pennsylvania, and Indiana University School of Medicine, Indianapolis, Indiana, US, respectively, noted that gallstone formation increased in the UDCA 300 mg and placebo groups following treatment cessation. [JAMA Surg 2020;doi:10.1001/jamasurg.2020.1527]
This highlights the importance of long-term follow-up and suggests that treatment cessation at 1 year may be premature. “[Identifying] characteristics of the patients who developed gallstones would be helpful in choosing the dose of UDCA,” they added.
While prophylactic UDCA in patients with gastric cancer undergoing gastrectomy is a fitting option, cholecystectomy remains an option for patients with a good cancer prognosis, they said.