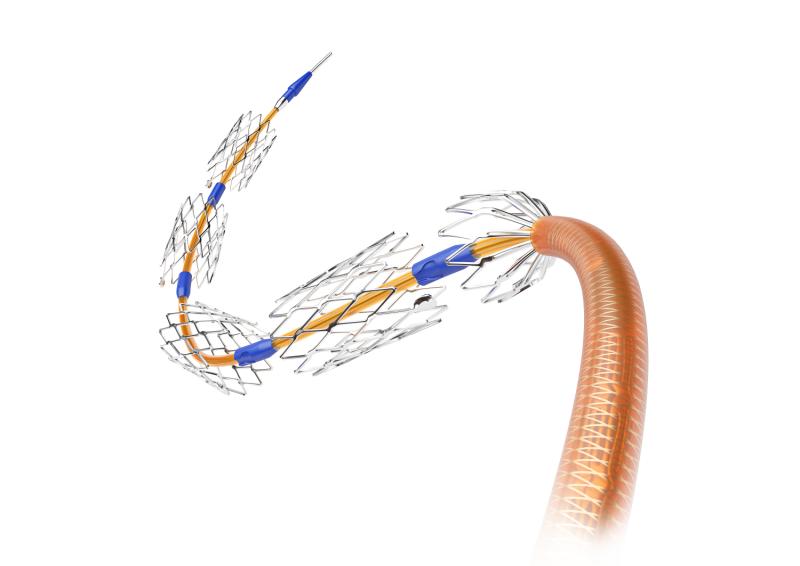
 VascuFlex® Multi-LOC is an innovative multiple stent delivery system (MSDS) for the treatment of peripheral artery disease (PAD)
VascuFlex® Multi-LOC is an innovative multiple stent delivery system (MSDS) for the treatment of peripheral artery disease (PAD)Zotarolimus- (ZES) and sirolimus- (SES) eluting stents have comparable long-term performance in diabetic and nondiabetic individuals, a new study has shown.
Researchers randomly assigned patients to receive either ZES (n=1,162) or SES (n=1,170). Stratifying by diabetes status showed that in the respective treatment subgroups, 169 and 168 had diabetes. Study endpoints included a composite of death and myocardial infarction, as well as the individual outcomes of death, myocardial infarction and revascularization.
Among those without diabetes, 348 and 341 patients in the ZES and SES groups, respectively, developed the primary composite endpoint. The corresponding incidence rates were 35.2 percent and 34.4 percent, representing a nonsignificant difference in risk (odds ratio [OR], 1.04, 95 percent confidence interval [CI], 0.86–1.25; p=0.69).
Disaggregating according to endpoint components yielded similar results (death: OR, 1.13, 95 percent CI, 0.93–1.39; p=0.22; myocardial infarction: OR, 0.80, 95 percent CI, 0.61–1.05; p=0.12). The likelihood of revascularization was likewise comparable between nondiabetics in either group (OR, 0.81, 95 percent CI, 0.61–1.09; p=0.17).
Similar trends were reported in diabetics. Those who were given ZES vs SES, for example, showed comparable rates and risks of the primary composite outcome (45.0 percent vs 50.3 percent; OR, 0.81, 95 percent CI, 0.53–1.24; p=0.33). The same was true for the individual components (death: OR, 0.80, 95 percent CI, 0.51–1.25; p=0.33; myocardial infarction: OR, 1.07, 95 percent CI, 0.60–1.91; p=0.81).
Notably, those who received ZES were at a significantly greater risk of revascularization (OR, 1.93, 95 percent CI, 1.05–3.66; p=0.078), though researchers noted that this may not be clinically driven.